News
-
TPC Partners with Junum for Malnutrition Clinical Decision Support
January 16, 2025NEW ORLEANS, LA, January 16, 2025 (EZ Newswire)– Junum, an innovative digital health company, is excited to announce a new partnership with TPC, bringing its cutting-edge MalnutritionCDS™ clinical decision support solution to enhance patient care and optimize reimbursement across TPC’s Member hospitals. This collaboration is a direct result of Junum’s remarkable success at Midland Memorial Hospital in West Texas, where the implementation of MalnutritionCDS™ generated a 3x return on investment (ROI) and new revenue in just 90 days.
Toni Goodson, Vice President of Performance Improvement at TPC, shared her enthusiasm about the partnership, stating, “After seeing firsthand how Junum’s solution delivered measurable improvements in care and reimbursement at Midland Memorial Hospital, we felt compelled to propose this transformative tool to the rest of our Member hospitals.”
Junum’s MalnutritionCDS™ is designed to help dietitians and physicians more accurately diagnose and treat malnutrition, ensuring better patient outcomes and more appropriate reimbursement through evidence-based decision-making and documentation. By integrating seamlessly into existing clinical workflows, the platform empowers care teams to identify and address malnutrition early, reducing complications and optimizing resource utilization.
“We are proud to expand our partnership with TPC and bring the benefits of MalnutritionCDS™ to a broader network of hospitals,” said Molly Hegarty, CEO of Junum. “Our solution has proven to drive both clinical and financial improvements, and we look forward to working closely with TPC to enhance patient care across Texas and Arkansas.”
For more details, read the press release here.
About Junum
Junum is a leading digital health company focused on developing innovative solutions that improve patient care and outcomes. Its flagship product, MalnutritionCDS™, offers healthcare providers a powerful tool to identify, diagnose, and manage malnutrition, driving better clinical decisions and improving reimbursement outcomes. For more information about Junum’s MalnutritionCDS™ and its impact on healthcare systems, visit junum.io or contact info@junum.io.
About TPC
TPC is a Member-driven coalition of independent community hospitals committed to achieving better outcomes together. By working through a committed platform, TPC drives collaboration and innovation across a range of clinical, operational and economic areas enabling providers to maximize the financial and non-financial value they receive. TPC empowers its Members to navigate the complexities of healthcare while maintaining their independence. For more information, visit www.tpc1.com, or follow us on LinkedIn.
References:¹ Guenter P, Abdelhadi R, Anthony P, et al. Malnutrition diagnoses and associated outcomes in hospitalized patients: United States 2018. Nutr. Clin Pract. 2021 [https://doi.org/10.1002/ncp.10771](https://doi.org/10.1002/ncp.10771)
2. *Hunger in Texas*. (n.d.). Feeding Texas. Retrieved September 11, 2023, from [https://www.feedingtexas.org/learn/hunger-in-texas/](https://www.feedingtexas.org/learn/hunger-in-texas/) -
Malnutrition Awareness Week 2024: Midland Memorial Hospital Quality Improvement
September 18, 2024September 16-20, 2024
Malnutrition Awareness Week 2024 - EDUCATE. EMPOWER. ELIMINATE.Malnutrition Awareness Week is an annual, multi-organizational campaign created by the American Society for Parenteral and Enteral Nutrition (ASPEN) to spotlight nutrition’s vital role in health and recovery and to educate the public on the importance of discussing their nutrition status with their healthcare professionals, especially when they are hospitalized.
Overcoming Challenges Around Hospital Malnutrition
A year ago in September, Midland Memorial Hospital went live with Junum’s Malnutrition Clinical Decision Support solution, MalnutritionCDS™ to help identify, diagnose and treat patients who are malnourished or at risk of malnutrition. So in recognition of Malnutrition Awareness Week 2024, we check back in with Kaitlyn Greb, MHA/MBA, RD LD, Director of Food and Nutrition Services at Midland to look back at their implementation and celebrate their success.
Midland Memorial Hospital more than tripled their malnutrition diagnosis rate from the previous year. Dietitians worked together to document malnutrition consistently using evidence-based guidelines, contributing to improved provider communication and enhanced reporting capabilities. By increasing alignment between the dietitians and the provider documentation, it is facilitating stronger communication between providers when making plans for patient care.
Passionate leaders like Kaitlyn and the dietitians at Midland Memorial Hospital and campaigns such as Malnutrition Awareness Week help us focus on nutrition as a patient right and its vital role in health and recovery. Put together with improved workflows, we can address the poor outcomes associated with unrecognized and untreated malnutrition. Malnutrition Awareness Week serves as a reminder of the devastation that undetected malnutrition can cause for patients and families. However, inspiring stories such as at Midland Memorial Hospital can help motivate other nutrition leaders to create change to reduce the frequency of undiagnosed malnutrition in their hospitals.
For more about Kaitlyn and Midland Memorial Hospital - Read the Case Study
You can learn more about about how Junum helps hospitals enhance their malnutrition care programs using technology by visiting our website, junum.io or contacting us at sales@junum.io.
-
Midland Health Partners with Junum to Improve Malnutrition Care
September 20, 2023Midland Memorial Hospital has partnered with Junum to help identify, diagnose and treat patients who are malnourished or at risk of malnutrition. Junum’s Malnutrition Clinical Decision Support solution, MalnutritionCDS™, is Junum’s flagship product and delivers key nutrition insights for physicians and dietitians caring for malnourished patients. The software is integrated directly within Midland’s Cerner electronic medical record, helping organize information and inform clinical decisions as early as possible. The software helps dietitians document clinical findings of malnutrition to support physicians’ diagnoses, so they can visualize treatment impact and intervene sooner.
“Malnutrition is not just a condition; it’s a silent saboteur of patient care. Malnutrition slows healing and recovery and can cause patients to experience longer hospital stays, higher costs, and increased risk of mortality. With Junum, our registered dietitians will bring malnutrition into focus for our providers. Together, we are committed to guaranteeing that every patient receives compassionate care tailored to their unique needs,” explains Kaitlyn Greb RD, LD, Director of Food and Nutrition at Midland Memorial Hospital.
Molly Hegarty, MS, RDN, Founder and CEO of Junum echos, “Junum is excited to partner with Midland Health to drive awareness for malnutrition and provide clinicians with the tools to improve care for this vulnerable population.”
Malnutrition Awareness Week 2023 - Nutrition Care is a Patient Right
Malnutrition Awareness Week is an annual, multi-organizational campaign created by the American Society for Parenteral and Enteral Nutrition (ASPEN) to spotlight nutrition’s vital role in health and recovery and to educate the public on the importance of discussing their nutrition status with their healthcare professionals, especially when they are hospitalized. Not only is malnutrition in patients a serious health concern that delays healing and recovery, but also costly as hospital costs for patients with malnutrition are 73% higher than for those who are not malnourished.
Addressing Food Insecurity Inside and Outside the Hospital
In Texas, 13% of Texas households — 1 in 8 Texans — experience food insecurity (Hunger in Texas, n.d.), which can put individuals at higher risk for malnutrition and its comorbidities. When hospitals can accurately diagnose malnutrition and recognize food insecurity during a patient’s hospital stay, they can provide referrals to programs like food banks, meal delivery services or nutrition education programs — helping to improve their health for years to come.
About Junum
Junum is founded and led by Molly Hegarty, a Registered Dietitian and engineer. The company helps hospitals understand and address malnutrition to maximize the value of their clinical teams, drive revenue and deliver exceptional patient care. Our intuitive tools operate within existing EHR workflows, giving clinicians easy access to the nutrition insights they need to drive improved outcomes. Visit junum.io for more information.
About Midland Health
Midland Health is a system of healthcare providers in Midland, Texas, with Midland Memorial Hospital at the center of their operations. Since 1950, Midland Memorial Hospital has exemplified excellence in patient care, medical education and community service. The mission and vision to lead healthcare for greater Midland and make Midland the healthiest community in Texas was established with the creation of Midland Health in 2014, expanding the healthcare footprint and impact through a coordinated system of providers. As Midland Memorial Hospital, a not-for-profit with 546 licensed beds, drives much of the work, the guiding principles behind Midland Health show a commitment to improving the community by reinvesting volunteered time and finances into the health of west Texas.
To learn more about Midland Health, visit midlandhealth.org.
References:¹ Guenter P, Abdelhadi R, Anthony P, et al. Malnutrition diagnoses and associated outcomes in hospitalized patients: United States 2018. Nutr. Clin Pract. 2021 [https://doi.org/10.1002/ncp.10771](https://doi.org/10.1002/ncp.10771)
2. *Hunger in Texas*. (n.d.). Feeding Texas. Retrieved September 11, 2023, from [https://www.feedingtexas.org/learn/hunger-in-texas/](https://www.feedingtexas.org/learn/hunger-in-texas/) -
Audit-Proof Your Malnutrition Documentation: An Interdisciplinary Approach
September 07, 2023In the world of medical coding, payer denials are a fact of life. The Association of Clinical Documentation Integrity Specialists (ACDIS) recently shared that malnutrition is among the top three most-denied diagnoses (surpassed only by sepsis and respiratory failure). As they point out in their Clinical Validation and Denials Management Council Report, all these conditions can be supported by multiple criteria sets — like GLIM and ASPEN, in the case of malnutrition.
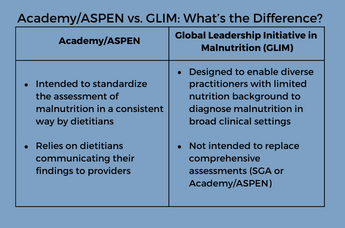 Unfortunately, there is no universal definition of malnutrition that definitively translates to an ICD-10 code — and that means payers may “cherry-pick” criteria from different frameworks to support denials. While this challenge isn’t going away any time soon, there are ways to prepare your teams for audits and minimize denials. We’ve gathered up a few places to start.
Unfortunately, there is no universal definition of malnutrition that definitively translates to an ICD-10 code — and that means payers may “cherry-pick” criteria from different frameworks to support denials. While this challenge isn’t going away any time soon, there are ways to prepare your teams for audits and minimize denials. We’ve gathered up a few places to start.
1. Align Your Cross-Functional Teams on Academy/ASPEN Criteria
We begin with a focus on consistency. If your medical and CDI team members are using different criteria — or even using the same criteria with varying levels of rigor or specificity — you may have a difficult time justifying your diagnoses. So the first step is to gather your medical and CDI teams to align on one criteria to use, and train on how to use it most effectively. (In fact, training is so important that we’ll come back to it later in this list.)2. Formalize and Document Your Policy
Once your medical and CDI teams are aligned and consistently using the criteria, it’s time to codify it and get approval from your Medical Review Committee (or local equivalent). By documenting your criteria, including the rationale and approvals behind those decisions, you will be in a strong position if (ok, when) you receive a query or denial from a payer.
Remember: do not change your clinical practices or definitions with the goal of aligning with payers. They may reference different criteria to question your diagnoses — but if you can point to a documented procedure that is followed consistently and has been properly validated, you can proceed with confidence3. Document Your Interventions
“If it’s not documented, it didn’t happen.” – Every regulatory agency inspector ever*
In addition to documenting findings of malnutrition and the appropriate severity level, it’s important to list all treatments and interventions to address the issue — regardless of who ordered them. This should include monitoring and follow-up plans to ensure your reimbursements reflect the level of care and length of stay required to treat the malnourished patient.4. Train and Assess Competencies Annually
Regular training is essential for both new hires and long-term team members. Growing workloads and frequently changing regulations can lead to inconsistency on even the best-managed teams. Training should include:* Roles and responsibilities
* Workflows from screening through coding
* Nutrition-focused physical exam
5. Open the Lines of Communication Between Medical Providers
Dietitians cannot diagnose malnutrition. Physicians don’t always recognize the signs and symptoms. Coders may be ill-equipped to spot and query every finding of malnutrition after the fact. Relieve the burden on your CDI teams and streamline your nutrition care workflows by facilitating communication between medical providers.Automated EHR workflows can go a long way here. Solutions like our MalnutritionCDS™ app make it easy for dietitians to document findings of malnutrition in the EHR, triggering the proper physician workflows in real time — with proper communication and documentation happening along each step of the process.
6. Automate Your EHR Workflows (With a Little Help from IS)
A technology-supported process can help prevent misses and streamline clinical validation. For example, when a dietitian documents findings consistent with malnutrition in the patient record, the physician can be flagged to review and make the diagnosis as appropriate. When your team can rely on easy-to-access technology to automate these processes for them, they can be confident they won’t miss a step. Ask your IS/IT team for help connecting the right applications to your EHR.7. Ask an Informaticist to Check Your Terminology
When it comes to data interoperability and quality reporting, words matter. Reach out to nutrition informatics experts to ensure your terminology (eNCPT, SNOMED, LOINC) can be appropriately mapped. Not only can it help you avoid denials — it can also help you support consistent and structured data management to help track the clinical effectiveness of nutrition interventions.Unfortunately, payer denials for malnutrition aren’t likely to go away any time soon. But with sound protocols, regular training and a little help from technology, you can spend less time worrying about them, and more time caring for your patients. We’re here to help. Get to know our MalnutritionCDS™ solution then reach out to explore how we can help you elevate clinical nutrition and drive results at your hospital.
-
Ochsner Health Blazes a Trail to Better Malnutrition Diagnosis with Junum
July 05, 2023Junum’s MalnutritionCDS™ solution integrates seamlessly with Ochsner’s leading EHR system
RELEASE DATE: July 5, 2023
NEW ORLEANS, La. – Junum, an innovative digital health company, today announced that Ochsner Health will integrate the Junum MalnutritionCDS™ clinical decision support solution with its Epic EHR. The technology innovation partnership aims to help Ochsner clinicians identify and diagnose malnutrition within their existing workflows for better patient care.
Nutrition Insights — When and Where Clinicians Need Them
The MalnutritionCDS solution, Junum’s flagship product, has proven valuable to Ochsner clinicians by delivering key nutrition insights directly to the EHR — helping organize information and inform clinical decisions as early as possible. The software also helps dietitians document clinical characteristics to support physicians’ diagnoses, as well as visualize treatment impact.
Addressing Food Insecurity Inside and Outside the Hospital
According to the U.S. Department of Agriculture, 14.5% of Louisiana residents face food insecurity, which can put individuals at higher risk for malnutrition and its comorbidities. When hospitals can accurately diagnose malnutrition and recognize food insecurity during a patient’s hospital stay, they can provide referrals to programs like food banks, meal delivery services or nutrition education programs — helping to improve their health for years to come.
“Junum and Ochsner Health share a passion for improving lives and communities through better care,” says Molly Hegarty, MS RDN, Founder and CEO of Junum. “With our MalnutritionCDS solution, we can put nutrition care insights in front of Ochsner’s care teams earlier than was previously possible. That means they can intervene sooner to help drive better outcomes in the hospital and beyond. We’re looking forward to many more success stories as this partnership progresses.”
“Malnutrition is not always obvious to physicians or top of mind when it comes to care, so having decision support tools and supporting information is incredibly helpful,” said Amanda Logue, MD, Chief Medical Officer at Ochsner Lafayette General.
Ochsner Health is an investor in the Healthcare Innovation Fund that invested in Junum in 2019.
See the press release here
Media inquiries, please email sales@junum.ioAbout Junum
Junum is founded and led by Molly Hegarty, a Registered Dietitian and engineer. The company helps hospitals understand and address malnutrition to maximize the value of their clinical teams, drive revenue and deliver exceptional patient care. Our intuitive tools operate within existing EHR workflows, giving clinicians easy access to the nutrition insights they need to drive improved outcomes. Visit https://junum.io for more information.
About Ochsner Health
Ochsner Health is an integrated healthcare system with a mission to Serve, Heal, Lead, Educate and Innovate. Celebrating more than 80 years of service, it leads nationally in cancer care, cardiology, neurosciences, liver and kidney transplants and pediatrics, among other areas. Ochsner is consistently named both the top hospital and top children’s hospital in Louisiana by U.S. News & World Report. The not-for-profit organization is inspiring healthier lives and stronger communities through its Healthy State by 2030 initiative, a bold and collaborative plan to realize a healthier Louisiana. Its focus is on preventing diseases and providing patient-centered care that is accessible, affordable, convenient and effective. Ochsner Health pioneers new treatments, deploys emerging technologies and performs groundbreaking research, including 4,000 patients enrolled in 685 clinical studies in 2022. It has more than 37,000 employees and over 4,700 employed and affiliated physicians in over 90 medical specialties and subspecialties. It operates 46 hospitals and more than 370 health and urgent care centers across Louisiana, Mississippi, Alabama and the Gulf South; and its cutting-edge Connected Health digital medicine program is caring for patients beyond its walls. In 2022, Ochsner Health treated more than 1.4 million people from every state and 62 countries. As Louisiana’s top healthcare educator of physicians, Ochsner Health and its partners educate thousands of healthcare professionals annually. To learn more, visit Ochsner.
-
RDNs on the Road: Focusing on What Matters at CNM Symposium 2023
May 15, 2023The 2023 CNM Symposium was held April 27-29 in Raleigh, NC. Now that we’ve finished unpacking our bags and catching up on sleep, we can finally process (and share) everything we learned at the conference.
It was a rewarding and refreshing few days talking with the clinical management community about the things that matter most right now. When it comes to improving health outcomes and elevating the importance of nutrition care, we walked away with three key takeaways:
1. Structured Data, Interoperability and Quality Reporting Matter
We know nutrition data is often documented and organized differently across health systems — and even across individual hospitals. So it was exciting to hear about advances being made to support consistent and structured data management to help track the clinical effectiveness of nutrition interventions.
Presenters shared how standardized charting with discrete fields using consistent terminology mappings to coded values supports interoperability, or the ability to share data both within and between systems. But it’s also the foundation for the move to electronic clinical quality measures (eCQM) reporting — which will be needed for the new Global Malnutrition Composite Score. Speaker Sandra Miller noted that “eCQM data can’t be reported if the ‘system’ can’t find it.” So be sure that includes all your screening and assessment results with date/time stamps in the record.
Unsure where to start... Consider performing a gap analysis and collaborating with a multidisciplinary team including quality and data analysts, clinical informatics, coders and IT, as well as clinicians.
We heard how structured nutrition data is being collected for registry research studies that will help illustrate the long-term impact of nutrition care. And importantly, plans were shared to add Fast Healthcare Interoperability Resources (FHIR) data exchange capabilities between ANDHII and EHRs — which will make it easier for RDNs to collect data on outcomes research and track and submit quality measures for reimbursement. It’s an exciting time to work in Clinical Informatics, and it’s gratifying to see the latest technical innovations to help support our missions.2. Medically Tailored Meals Matter
One particularly interesting session shared the experience of running Medically Tailored Meal programs, and the evidence backing up their importance. In these programs, home-delivered meals are prepared under RD supervision to meet an individual or population’s unique nutritional needs. They have been shown to improve nutrition and overall health, reduce hospital readmissions and reduce hospital length of stay. It was a wonderful discussion, and an important reminder of the importance of nutrition care every day — not just when people are in the hospital.3. Diversity, Equity and Inclusion Matter
The dietetics field is no stranger to a lack of diversity. As one session pointed out, ~80% of dietetics professionals are white, and the situation doesn’t seem to be improving. In fact, the past 18 years have seen an 11.6% decrease in the number of black dietetic students and interns. It’s clear our industry needs to prioritize diversity, equity and inclusion. While we focus on helping our patients, we also need to question our status quos. That means examining our own biases and creating opportunities to welcome underrepresented groups into our field. Greater inclusivity in our profession will help us fight those biases and improve health equity in all the populations we serve.When returning from a conference, there is never a shortage of work to be done. But conferences like CNM Symposium are so important to helping us connect, share learnings and focus our efforts where the need is greatest. We enjoyed connecting with many of you there. And if we missed you, we hope you’ll reach out to talk with us about the nutritional needs in your organization.
-
CMS Global Malnutrition Composite Score: Are You Ready to Report?
April 26, 2023Nutrition care matters — and the healthcare industry is taking notice. That’s why, last year, the Centers for Medicare and Medicaid Services (CMS) adopted the Global Malnutrition Composite Score (GCMS) electronic clinical quality measure (eCQM) into its Hospital Inpatient Quality Reporting program.
The goal is clear: to help improve outcomes by devoting more attention to patients’ nutritional needs and related social determinants of health — particularly for those most at risk for nutritional deficiency and food insecurity.
While the reporting will be voluntary, CMS is keen to have this data — and for good reason. One in three hospitalized patients in the US are malnourished or at risk, yet less than 8.9% are officially diagnosed.¹ This frequently missed diagnosis negatively impacts patient outcomes and drives up the cost of care. And it affects many of your most vulnerable populations, including those over 65 years of age.²
What Goes Into the GMCS Measure? The measure consists of four key components:
1. Screening
Screen for malnutrition risk at admission.2. Nutrition Assessment
Complete nutrition assessments for patients identified as at-risk for malnutrition.3. Document Malnutrition Diagnosis
Appropriately document malnutrition diagnoses for patients identified with malnutrition.4. Develop Nutrition Care PlanDevelop a nutrition care plan for malnourished patients, including recommended treatment plan.
Why Should You Start Preparing to Report Malnutrition Data Now?
The GMCS reporting period begins in January 2024, but many hospitals are already beginning preparations. Here are a few steps you can take now to prepare:
Assess Your Readiness
Do you have the data you’ll need? How easy is it to access? How could the process be streamlined?Enhance Your EHR
If nutrition care isn’t adequately documented today, investigate options to improve documentation without overburdening your dietitians or physicians.Do a Data Quality Check
Consult with clinical teams, nutrition teams and CDI teams. If you’re seeing frequent denials relating to malnutrition, now is the time to get to the root cause.How Can Junum Help?
Our MalnutritionCDS™ solution helps RDs document the clinical evidence supporting physicians’ malnutrition diagnoses — helping to inform nutrition care plans, maximize hospital reimbursements and avoid denials. It provides the malnutrition quality data and analytics you’ll need for GMCS reporting, with at-a-glance scorecards making the data easy to organize and interpret.
The Time is Now
Why wait until next year to tap into the rewards of quality malnutrition care and reporting? It pays to be an early adopter. Start now and meet CMS quality reporting requirements, maximize Medicare payments and help advance health equity by improving malnutrition care performance.And remember — we’re here to help. Learn more at https://junum.io, then reach out to get started.
References:¹ Based on 2018 HCUP data. Guenter P, Abdelhadi R, Anthony P, et al. Malnutrition diagnoses and associated outcomes in hospitalized patients: United States 2018. Nutr. Clin Pract. 2021 https://doi.org/10.1002/ncp.10771
2. Sheean P, Farrar IC, Sulo S, Partridge J, Schiffer L, Fitzgibbon M. Nutrition risk among an ethnically diverse sample of community-dwelling older adults. Public Health Nutr. 2019 Apr;22(5):894-902. doi: 10.1017/S1368980018002902. Epub 2018 Nov 6. PMID: 30396375; PMCID: PMC6521784 -
Building Better Health Equity with Inpatient Malnutrition Programs
February 07, 2023If you work in a hospital, you’re aware of the myriad of health challenges that face your patients. With so many severe injuries and illnesses to address, things like malnutrition and food insecurity tend to be left to the margins — but these are problems that can have a significant impact on a patient’s health. The systemic lack of recognition for malnutrition is not only affecting the health needs of individual patients, but it also contributes to the widening gap of health disparities in our communities.
When patients are discharged, it can be difficult to know how their circumstances effect the continuation of their recovery. One of the key benefits of a strong inpatient malnutrition program is that it provides a bridge between inpatient treatment and the patient’s wider community and support programs. By diagnosing malnutrition and recognizing food insecurity during a patient’s hospital stay, you can provide referrals to programs that can help address these issues in the long term. This can include programs like food banks, meal delivery services, and nutrition education programs.
Of course, medical professionals know that there are “social determinants of health” like food insecurity, and do their best to address them when possible. However, these issues can be difficult to diagnose, especially when clinician bandwidth is limited. Many patients may not be aware of their own nutritional status or may not be willing to disclose information about their eating habits. Rather than expecting patients to self-diagnose, hospitals can glean insight into an individual’s nutritional status by implementing a comprehensive screening process, which can include questions about food insecurity, dietary habits, and weight changes. This information can then be used to make informed decisions about the best course of action.
In addition to addressing malnutrition and food insecurity, a strong inpatient malnutrition program can also provide benefits to the hospital and healthcare system as a whole. Patients who are well-nourished are more likely to have better health outcomes, faster recoveries, and lower healthcare costs. A malnutrition diagnosis turns into community support for the patient, which in turn leads to better quality of diet, stronger ability to adhere to outpatient care plans, and fewer hospital readmissions. A study at New Hanover demonstrated a 24% lower readmissions rate after just one year of implementing a malnutrition transition-of-care program for at-risk individuals.
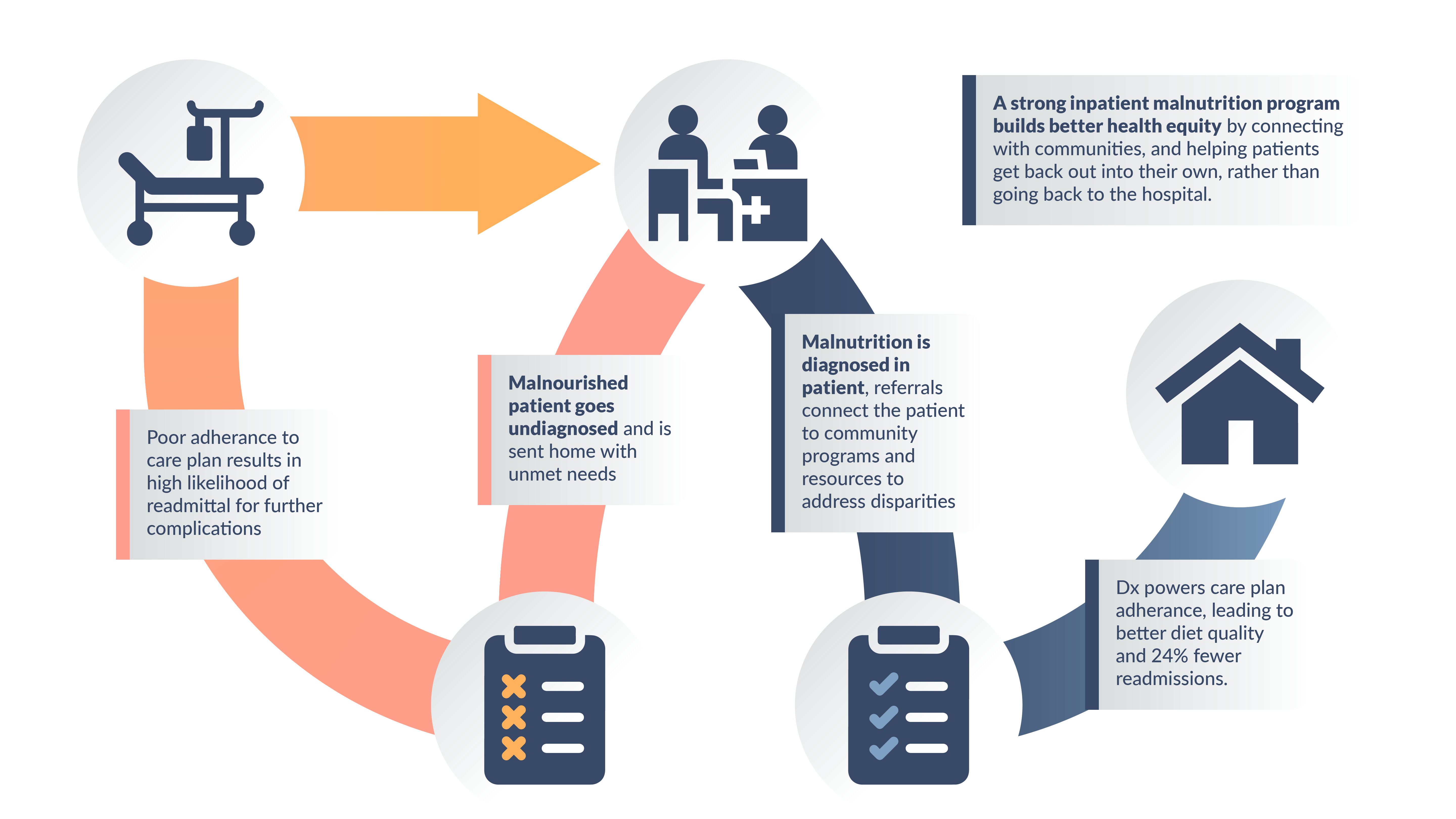
Health disparities are an irrefutable issue, and it is crucial for healthcare providers to take an active role in mitigating these disparities by looking for and addressing their root causes. Clinical Decision Support (CDS) platforms like Junum are the key to healthier communities and more efficient care centers. With Junum, patients can get the support they need to change their own health trajectory, rather than getting stuck in a loop of hospitalization and disconnected discharge. And it all happens without distracting clinicians and administrators from the amazing work they do to keep their facilities running smoothly. We can help build better health equity for your patients and ensure that everyone has access to the resources they need to maintain good health — learn more at https://junum.io.
-
Could “Severity of Illness” Impact Your Hospital’s Bottom Line?
January 09, 2023By Molly Hegarty, MS RDN
Malnutrition is a frequently missed diagnosis that can negatively impact hospital revenue. In previous blog posts, we’ve outlined how undocumented malnutrition leaves payments on the table, but a technology-driven, multidisciplinary approach to screening, assessing and documenting a secondary diagnosis of malnutrition can result in higher hospital reimbursements.
Under the Medical Severity-Diagnosis Related Group (MS-DRG) system used by the Centers for Medicare and Medicaid Services (CMS) for hospital payments for Medicare beneficiaries, malnutrition may qualify as a either a major complication/co-morbidity (MCC) or complication/co-morbidity (CC) thereby increasing the base level reimbursement for the primary diagnosis. However, hospitals routinely rely on another classification system, the All Patient Refined DRG (APR-DRG) developed by 3M, to determine the most accurate assessment of the patient’s severity of illness (SOI) and risk of mortality (ROM). So it’s important to understand how diagnosing malnutrition fits into this model.
What is SOI and How Does it Impact Hospital Reimbursement?
Severity of Illness or SOI, refers to the extent of physiologic decompensation or organ system loss of function. Plainly, SOI is a measure of how sick a patient is, based on their clinical condition, functional status among other factors. Some payors, including many state Medicaid programs, opt to use the AP-DRG method to classify hospital inpatient stays into clinically meaningful diagnostic groups which will determine the amount the hospital gets paid for a given condition regardless of actual length of stay. But unlike the MS-DRG system in which reimbursement is driven by the primary diagnosis and the existence of only one CC or MCC, APR-DRGs take into consideration all secondary diagnoses and procedures that impact the complexity of the patient’s situation including age, gender, risks and expected course of treatment. In this method, hospital payments will be adjusted based on the resulting impact of the SOI level, so it is critical to document all of the patient’s contributing conditions. If malnutrition goes undocumented and undiagnosed, then the true picture of the patient’s SOI will be underestimated.
In general, every complete inpatient stay is assigned to a single DRG using a computerized algorithm that considers the patient’s diagnoses, age, procedures, and discharge status. Each DRG has a relative weight that reflects the typical hospital resources needed to care for a patient in that DRG relative to the hospital resources needed to care for the average patient. SOI can be calculated using the All Patient Refined Diagnosis Related Groups (AP-DRG) system algorithms. SOI scores are based on all comorbidities (like malnutrition) and are stratified into four levels: 1. Minor, 2. Moderate, 3. Major, and 4. Extreme. Each patient encounter is then assigned to one of the four levels based on the number, nature, and interaction of complications and comorbidities. Higher severity levels will trigger higher payments due to the increased expected cost of caring for these complex patients. So a secondary diagnosis of protein-calorie malnutrition may affect the overall SOI for the patient. Payment would increase based on the shift in the APR relative weight for this case. See the example below to see the extent of this effect.
Comparison of Impact of Severe Malnutrition on AP-DRG Severity of Illness, Relative Weight and Hospital Reimbursement Revenue
Base AP-DRG Group 194 (heart failure) 194 (heart failure) Primary Diagnosis Congestive Heart Failure (CHF) Congestive Heart Failure (CHF) Secondary Diagnosis • Chronic Obstructive Pulmonary Disease (COPD)
• Atrial Fibrillation• Chronic Obstructive Pulmonary Disease (COPD)
• Atrial Fibrillation
• Severe Protein Calorie Malnutrition
• Decubitus UlcerSeverity of Illness (SOI) 2 4 Risk of Mortality (ROI) 2 4 APR relative weight 0.7035 2.3149 Estimated Reimbursement (Given an average DRG base rate of $6000) $441.00 $16,204.30 Source: Adapted from CDI Strategies, Volume 12, Issue 4, 2018. https://acdis.org
Tracking Quality Improvement & UtilizationBeyond payment, hospitals further use these AP-DRG SOI and ROM factors to track and compare quality and resource utilization, as well as to generate health status risk scores that health plans and payors use to predict costs for healthcare services. These factors help healthcare providers determine the appropriate level of care for each patient, and can also be used to help predict outcomes and guide critical treatment decisions. SOI can also serve as a targeting system that helps clinical facilities reach KPIs and reduce unnecessary resource expenditures.
According to 2018 data from The Agency for Healthcare Research and Quality, malnutrition affects more than 30% of hospitalized patients, but only 8.9% received a coded malnutrition diagnosis upon discharge. As discussed in this ASPEN video overview of a study published in Nutrition in Clinical Practice, malnourished patients are at much higher risk for poor health outcomes, require significantly longer hospital stays and are more likely to be readmitted. If you compare patients with malnutrition to those without a diagnosis of malnutrition, you see just how big an impact malnutrition has in terms of cost and outcomes:
- Longer length of stay: 9.0 days vs 4.7 days
- Higher in-hospital mortality: 3.4 times higher
- Higher hospital costs: $9,969 more per stay
- Higher readmission rates: 89.2% vs 77.2%
Junum helps hospitals address malnutrition so they can maximize the value of their clinical teams, drive revenue and deliver better patient care. Junum’s MalnutritionCDS™ software improves clinical workflows, saves physicians time, and helps CDI and Coding teams more accurately determine a patient’s true severity. As one of our Client hospital physician leaders said, “the specificity of malnutrition metrics we are able to quantify [now with Junum] are a game-changer in calculating risk of mortality and severity of illness.”
By accurately assessing and documenting the severity of illness of their patients, hospitals can ensure that they are reimbursed appropriately for the care they provide. Accurate SOI can also help payors better understand the resource utilization and costs associated with treating complex cases. This can inform their decision-making and help them identify opportunities for cost containment and efficiency improvements.
Overall, tracking SOI in malnutrition cases is beneficial for hospitals, patients, and payors. It helps hospitals provide the best possible care to their patients, and it helps payors understand the costs and resource utilization associated with treating malnutrition cases. By working together, hospitals and payors can improve patient outcomes and control costs, ultimately benefiting the healthcare system as a whole.
At Junum, we help hospitals achieve better SOI accuracy and improved malnutrition care. Get an inside look at how our tools drive higher reimbursements by scheduling a demo at https://junum.io.
Sources:¹ All Patient Refined Diagnosis Related Groups (AP-DRGs): Methodology Overview. Version 20.0. 3M Health Information Systems; 2003. https://www.hcup-us.ahrq.gov/db/nation/nis/APR-DRGsV20MethodologyOverviewandBibliography.pdf ² Fernandes, et al. Does malnutrition influence hospital reimbursement? A call for malnutrition diagnosis and coding,Nutrition,Volume 74,2020,110750. https://doi.org/10.1016/j.nut.2020.110750. ³ Souza J, Santos JV, Canedo VB, Betanzos A, Alves D, Freitas A. Importance of coding co-morbidities for APR-DRG assignment: Focus on cardiovascular and respiratory diseases. Health Information Management Journal. 2020;49(1):47-57. doi:10.1177/1833358319840575 ⁴ Based on 2018 HCUP data. Guenter P, Abdelhadi R, Anthony P, et al. Malnutrition diagnoses and associated outcomes in hospitalized patients: United States 2018. Nutr Clin Pract. 2021. https://doi.org/10.1002/ncp.10771 -
12 Tips to Recharge Your Malnutrition Program
October 17, 2022Guest Post by Michelle Mathura, RDN, LD/N
Michelle is Director of DM&A’s Nutrition Division where she helps empower dietitians and clinical teams to improve their malnutrition care.To celebrate the important work being done in our industry related to malnutrition and highlight the advocacy efforts in support of the recent Malnutrition Awareness Week and [White House Conference on Hunger, Nutrition and Health, we share with you – the leaders, and you all are leaders– 12 important tips you can use to ramp up and keep the momentum going with your Malnutrition Programs!

MEASURE – It’s crucial for the success of your malnutrition program to measure your outcomes. Leaders must know their numbers. Data is key. You may ask, “What numbers should I know and how do I get them?” It’s important to track malnutrition prevalence, coded malnutrition diagnoses and nutrition diagnoses, and incremental revenue monthly. Check out the Global Malnutrition Composite Score (GMCS) electronic clinical quality measure to see if you can access data on all four components of the score. Then, understand what to do with this information. How else are you going to support the work you and your team are doing?
ALIGN – Align with interdisciplinary team members and departments to work on program objectives and goals. Working together will create efficiencies and provide the best patient care.
LEAD – The best way to teach, educate, and garner support for your program is to lead by example. Start with kindness, listening, resourcefulness, and providing the best practice tools and training your team needs to be successful and do their job.
NOTIFY– Is your facility using the best practice nutrition screening tool for your patient population? If not, screening is a great place to start. But don’t stop there. You can also leverage the latest clinical decision support technology to notify providers automatically when patients meet diagnostic criteria.
UNIFY – Bring your dietitian team together by getting everyone on the same page to provide best practice nutrition screening and assessment. Providing expert Nutrition Focused Physical Exam (NFPE) and Hand Grip Strength (HGS) onsite training for your team will ensure competency and confidence and the best and safest patient care!
TIME – The time is now! The reporting period for the new GMCS begins in January 2024. Examine your program and set some new goals. What goals are you still working on? What do you need to do to accomplish those goals by the end of 2022? Begin with one thing and ask yourself, “Is this realistic? What’s holding me back from accomplishing my goal?”
REIMBURSEMENT – It’s ok to talk about insurance reimbursement. Some people in leadership positions may not want to look at the “dollars” or on the flip side, they only want to look at the money coming in. Always be patient centered. Insurance reimbursement related to the coded diagnosis of malnutrition is important to patient care and should be monitored on a monthly basis. It’s a leader’s job to know their numbers, reimbursement is part of this.
IMPROVE – To grow is to learn and to learn is to grow. Learning happens through experience - classical learning, reading, and doing are some other examples. We all are “works in progress” as are the programs we lead. Look at your Malnutrition Program and your dietitian team – what is needed to get to the next best level?
TOOLS – Do you have the necessary tools to grow your malnutrition program and your dietitian team? Optimize your EHR with integrated apps that automate your workflows and audit-proof your documentation. NFPE and HGS training modules, quizzes, and competencies are key to success for any Malnutrition Program providing the best and safest patient care.
IDENTIFY – Identify key leaders within your dietitian team. Empower them with the best practice tools and training to lead this malnutrition initiative and keep the momentum going! Identify physician champions to support all your nutrition efforts, especially your malnutrition program.
ONSITE – Hands down, hands on onsite training is the best and most effective training there is for the NFPE and HGS! Onsite training for your dietitian team paired with an expert dietitian NFPE success coach working with their patients…. there’s nothing better than this to support the dietitian, provide the best and safest patient care, and ensure confidence and competence!
NOW – Now it’s time to take the next step! Start today. Pick one thing from this list and improve your program! Now is the time to light the fire and keep the flame burning!
Let us show you how to implement these 12 steps at your institution!
We offer free 30-minute consultations with our team of DM&A and Junum malnutrition care experts. Let us put our combined expertise to work for you.
Contact: nutritionpartners@destination10.com
-
Junum Wins HearstLab: Texas Pitch Competition Including $100,000 Prize
August 04, 2022Junum, an innovative digital health company, was awarded $100,000 from HearstLabs as a part of the HearstLab: Texas Pitch Competition
In the U.S., one in three patients admitted to the hospital is malnourished or at risk – but <8.9% are diagnosed. Junum’s clinician-driven technology is designed to help hospitals deliver exceptional patient care and maximize revenue by providing the tools needed to accurately diagnose malnutrition within existing EHR workflows. The software is currently being used by hospitals across the U.S. When malnutrition is properly diagnosed and coded, reimbursements can rise significantly. In fact, hospitals using Junum’s solution have nearly doubled their malnutrition diagnosis rates — and seen multi-year revenue increases as a result.
As a winner of Pitch HearstLab:Texas, Junum will receive a $100,000 investment and three months of hands-on support. HearstLab was founded in 2015 and is a part of Hearst, a leading global, diversified information, services, and media company with operations in 40 countries. HearstLab provides cash investment and support to early-stage women-led, tech-enabled startups in North America.
“Unrecognized malnutrition affects millions of hospitalized patients each year and our MalnutritionCDS solution helps physicians recognize and treat malnutrition quickly while also generating significant revenue for hospitals” said Molly Hegarty, founder and CEO. “We are honored to join the HearstLab portfolio in order to advance our mission to bring our nutrition-focused clinical decision support technology to more healthcare systems.”
Read the full press release from HearstLab here.
About Junum
Junum is founded and led by Molly Hegarty, a Registered Dietitian and a former Intel engineer. The company helps hospitals understand and address malnutrition to maximize the value of their clinical teams, drive revenue and deliver exceptional patient care. Our intuitive tools operate within existing EHR workflows, giving clinicians easy access to the nutrition insights they need to drive improved outcomes. Schedule a demo today at https://junum.io and check out Junum on Linkedin and Twitter.
About HearstLab
HearstLab provides cash investments and services to early-stage, women-led startups innovating across fintech, data analytics, health, transportation, enterprise technology and media. Its mission is to close the gap in VC funding for women by helping founders build sustainable and highly scalable businesses. With access to Hearst resources across 360+ businesses, HearstLab’s breadth of services includes assistance with privacy and security, software development, legal services, financial analysis, and marketing and design support. To learn more about HearstLab, visit HearstLab.com and connect with us on LinkedIn.
-
The Malnourished Patient Journey: Part 4 The Readmission
June 08, 2022By Samir Hussaini, MD
In the final part of our patient journey, the undiagnosed malnourished patient has unfortunately been hospitalized again, but now at a different hospital. Let us see how this encounter differs from the previous ones described.
The Role of the Dietitian
Dietitians are invaluable healthcare providers and are essential members of the inpatient care team. They are experts in medical nutrition therapy and provide nutrition assessments and tailored nutrition interventions. Dietitians also act as an education resource for patients when it comes to information and advice for nutrition. Dietitians tailor nutrition treatment plans (e.g., oral, parenteral, and enteral nutrition) and modify diets for disease states like heart failure and renal disease.The Patient
Mr. Doe* presented to the emergency department for evaluation after a fall. The emergency physician noticed generalized weakness and ulceration over the sacral area. The x-ray of the sacrum and coccyx showed a possible fracture. Lab work revealed hypokalemia and hypomagnesemia. Intravenous (IV) antibiotics and electrolyte supplementation were administered. The patient was admitted for recovery.During this admission, the hospitalist asked about the patient’s home situation. The patient mentioned he had been eating less and was relying on his daughter more for food preparation. The hospitalist noticed that he had been admitted for congestive heart failure (CHF) exacerbations five times in the past three months. The hospitalist also recognized that this patient was most likely malnourished and consulted the dietitian for assessment and recommendations. This consult to the dietitian was sent less than 24 hours after the patient was admitted.
The dietitian’s note included a malnutrition assessment that incorporated a nutrition-focused physical exam to identify any signs of depletion in different body regions, subcutaneous fat loss, and muscle loss. The dietitian’s recommended nutrition care plan included a cardiac diet and oral nutrition supplement prescription to be consumed twice a day. The oral food intake target was greater than 50% of all meals and oral nutrition supplements. The dietitian also provided diet education to the patient. The dietitian included in her note that she reviewed these recommendations with the nurse.
Subsequent progress notes by the hospitalist included a medical malnutrition diagnosis as well as tracking the nutrition interventions recommended by the dietitian. As the patient improved throughout his admission, the dietitian kept noting progress until discharge. The patient was counseled on nutritional goals to aim for after discharge.
This malnourished patient encounter shows a hospital better equipped at assessing and treating malnutrition. Nutrition interventions in the inpatient setting have been shown to reduce the length of stay by 2 days and reduce 30-day readmission rates by 27% (¹,²). The main issue in malnutrition care is the gap of patients that are malnourished but are not identified or have their needs fully addressed during their hospital admission.. The Malnutrition Quality Improvement Initiative (MQii), a proven toolkit for better identifying malnutrition, describes four electronic clinical quality measures (eCQMs) that are best practices for hospitals³. These eCQMs are the following:
- Completion of a malnutrition screening within 24 hours of admission
- Completion of a nutrition assessment for patients identified as at risk for malnutrition within 24 hours of a malnutrition screening
- Nutrition care plan for patients identified as malnourished after a completed nutrition assessment
- Appropriate documentation of a malnutrition diagnosis
Employing these practices have helped hospitals make malnutrition diagnosis and document nutrition interventions.
While it was unclear if this patient had a malnutrition screening on admission using a screening tool, this patient had a nutrition assessment completed by the dietitian within 24 hours of admission, a documented nutrition care plan, a medical malnutrition diagnosis in the progress notes, and nutrition intervention recommendations for post-discharge. All of these steps executed during this admission is setting this patient up for better overall outcomes and well-being.
Do you wonder if your hospital compares to best practices seen above when dealing with malnutrition in the inpatient setting? Take our Hospital Malnutrition Quality Survey (HMQS) to assess your organization’s malnutrition care program or schedule a demo https://junum.io. Otherwise you can learn more about about how Junum helps hospitals enhance their malnutrition care programs using technology by visiting our website, junum.io or contacting us at sales@junum.io.
*To protect the patient’s identity, names and initials have been changed.
References:¹ Pratt KJ, Hernandez B, Blancato R, Blankenship J, Mitchell K. Impact of an interdisciplinary malnutrition quality improvement project at a large metropolitan hospital. BMJ Open Qual. 2020 Mar;9(1):e000735. doi: 10.1136/bmjoq-2019-000735. PMID: 32213547; PMCID: PMC7170540. ² Sriram K, Sulo S, VanDerBosch G, Partridge J, Feldstein J, Hegazi RA, Summerfelt WT. A Comprehensive Nutrition-Focused Quality Improvement Program Reduces 30-Day Readmissions and Length of Stay in Hospitalized Patients. JPEN J Parenter Enteral Nutr. 2017 Mar;41(3):384-391. doi: 10.1177/0148607116681468. Epub 2016 Dec 6. PMID: 27923890. ³ Silver HJ, Pratt KJ, Bruno M, Lynch J, Mitchell K, McCauley SM. Effectiveness of the Malnutrition Quality Improvement Initiative on Practitioner Malnutrition Knowledge and Screening, Diagnosis, and Timeliness of Malnutrition-Related Care Provided to Older Adults Admitted to a Tertiary Care Facility: A Pilot Study. J Acad Nutr Diet. 2018 Jan;118(1):101-109. doi: 10.1016/j.jand.2017.08.111. PMID: 29274640. -
The Malnourished Patient Journey: Part 3 Discharge
April 26, 2022By Samir Hussaini, MD
After being treated for an exacerbation of congestive heart failure, Part 3 of our patient journey blog series takes the patient through the discharge process. Here, we can see some common pitfalls that may occur when discharging patients who are experiencing malnutrition or at risk for malnutrition.
The Role of the Dietitian
Dietitians are invaluable healthcare providers and are essential members of the inpatient care team. They are experts in medical nutrition therapy and provide nutrition assessments and tailored nutrition interventions. Dietitians also act as an education resource for patients when it comes to information and advice for nutrition. Dietitians tailor nutrition treatment plans (e.g., oral, parenteral, and enteral nutrition) and modify diets for disease states like heart failure and renal disease.The Patient
Mr. Doe* was discharged with home health care, as well as instructions for a cane, and follow-up with an advanced heart failure clinic. On admission, the nurse did not recognize a 6.5% weight loss, and waited to perform the MST 24 hours before discharge, leaving little room for nutrition intervention in the hospital setting. As a result, the dietitian was not consulted and a nutrition assessment and nutrition focused physical exam (NFPE) was not performed. This led to a missed opportunity for both a nutrition and medical based diagnosis of malnutrition, and the patient leaving the hospital without a nutrition care plan including nutrition interventions to follow at home.This patient most likely would have met criteria for a malnutrition diagnosis. Screening on admission would have identified this patient as already malnourished due to him suffering from an acute exacerbation of heart failure, a 6.5% weight loss within three months, and a BMI of 19.
Different organizations use different malnutrition classification criteria (e.g., the Academy/ASPEN, Merck, GLIM, etc.) and different malnutrition workflows leaving room for non-dietitian clinicians to not be properly trained or forced to use inefficient workflows or criteria. One way to identify and overcome gaps in malnutrition care includes, adoption of practices in the Malnutrition Quality Improvement Initiative (MQii) toolkit, a collection of evidence based best practice resources for malnutrition diagnosis, and optimizing the EHR to assist in the coordination of care. One study using the MQii toolkit led to a 100% RDN-based diagnosis of malnutrition when patients were screened and identified as malnourished or at high risk, and a 4.8% increase in documentation of malnutrition¹.
Once identified, communicating the diagnosis and nutrition interventions to the patient is vital. By doing this it increases the chance of patient buy-in that will lead to better adherence to treatment plans and carrying out medical recommendations from discharge in an outpatient capacity.
Malnourished older patients are often likely to reappear to the hospital for admission. Guenter et all found that 55% of malnourished patients that were readmitted within 30 days were older than 65². One large single center study of surgical patients saw that the third most common reason for readmission was failure to thrive/malnutrition³. Physicians that ignore malnutrition during the hospital admission are making patients susceptible to this concept of malnutrition medical frailty called Post-Hospital Syndrome leading to the high probability of readmission for these patients within 30 days⁴ Hopefully, we can continue the call-to-action as physicians to think about this demographic of older malnourished patients and ensure we are discharging them with some sort of nutrition care plan.
Identifying malnutrition and prescribing the correct nutritional intervention is vital. Even though this patient’s journey through this particular hospital stay did not result in correctly identifying the signs and symptoms of malnutrition, we will see in part 4, what it looks like when a malnourished patient is properly assessed and treated during a hospital visit.
What areas in this patient’s journey do you feel can be improved?
Junum’s MalnutritionCDS™ software improves clinical workflows, saves physicians time, and drives hospital revenue. Our intuitive tools operate within existing EHR workflows, giving clinicians easy access to the nutrition insights they need to drive improved outcomes. Junum’s MalnutritionCDS™ increases the quality of malnutrition care and drives new top-line revenue along with providing a KPI data driven scorecard to track progress.
*To protect the patient’s identity, names and initials have been changed.
References:
¹ Silver HJ, Pratt KJ, Bruno M, Lynch J, Mitchell K, McCauley SM. Effectiveness of the Malnutrition Quality Improvement Initiative on Practitioner Malnutrition Knowledge and Screening, Diagnosis, and Timeliness of Malnutrition-Related Care Provided to Older Adults Admitted to a Tertiary Care Facility: A Pilot Study. J Acad Nutr Diet. 2018 Jan;118(1):101-109. doi: 10.1016/j.jand.2017.08.111. PMID: 29274640. ² Guenter P, Abdelhadi R, Anthony P, Blackmer A, Malone A, Mirtallo JM, Phillips W, Resnick HE. Malnutrition diagnoses and associated outcomes in hospitalized patients: United States, 2018. Nutr Clin Pract. 2021 Oct;36(5):957-969. doi: 10.1002/ncp.10771. Epub 2021 Sep 6. PMID: 34486169. ³ Kassin MT, Owen RM, Perez SD, Leeds I, Cox JC, Schnier K, Sadiraj V, Sweeney JF. Risk factors for 30-day hospital readmission among general surgery patients. J Am Coll Surg. 2012 Sep;215(3):322-30. doi: 10.1016/j.jamcollsurg.2012.05.024. Epub 2012 Jun 21. PMID: 22726893; PMCID: PMC3423490. ⁴ Krumholz HM. Post-hospital syndrome--an acquired, transient condition of generalized risk. N Engl J Med. 2013;368(2):100-102. doi:10.1056/NEJMp1212324 -
DM&A and Junum Announce Partnership to Help Hospitals Take Action in Mitigating Malnutrition!
March 31, 2022For Immediate Release
Tuesday, April 5, 2022
DM&A and Junum announced today that they have entered a strategic partnership that will help hospitals take action to provide the best tools to care for malnutrition. Untreated malnutrition diagnoses put patients at risk for worse outcomes. By combining DM&A’s malnutrition education, training, and coaching expertise with the power of Junum’s MalnutritionCDS technology, we will help hospitals identify, diagnose, and treat malnutrition to improve patient care and optimize reimbursement. The accurate identification, intervention and documentation of malnutrition allows hospitals to be reimbursed for the resources required to care for the specific needs of these malnourished patients.
Matthew Miller, Chief Executive Officer at DM&A says: “We are excited to engage alongside Junum to help hospitals address the often-undiagnosed condition of malnutrition. We believe that Junum’s innovative technology perfectly complements our longstanding Malnutrition Education and Training Program that improves the quality of nutrition care in hospitals today.”
Molly Hegarty, MS RDN, Founder and CEO of Junum agrees saying, “We’re proud to partner with DM&A to deliver intuitive tools that operate within existing EHR workflows giving physicians and dietitians easy access to the nutrition insights they need to drive improved outcomes for malnourished patients.”
Media inquiries, please email sales@junum.io
About DM&A
The DM&A team is comprised of industry recognized leaders, ranging from Certified Executive Chefs, MBAs, PhDs, Registered Dietitians, Authors, Professional Speakers, and Executive Success Coaches, which allows us to offer a multitude of specialized services. This includes but is not limited to strategic planning, operational transformation, clinical nutrition support services, design services, hospital room service, senior dining operations, and interim staffing. Our mission it to greatly improve the experiences of patients, residents, and guests by enhancing the culture and operations of those that serve them.
info@destination10.com
www.destination10.comAbout Junum
Junum is an innovative digital health company on a mission to put nutrition at the forefront of healthcare using technology. Founded and led by Molly Hegarty, nutritionist and engineer, the company employs a team of experts in nutrition and healthcare informatics. Junum helps hospitals address malnutrition so they can maximize the value of their clinical teams, drive revenue and deliver exceptional patient care. For more information or to schedule a demo, visit www.junum.io today.MalnutritionCDS and Junum are trademarks or registered trademarks of RDF Technology, LLC.
-
Patient Journey Blog Part 2 - The Ward
March 07, 2022By Samir Hussaini, MD
The Role of the Hospitalist
The hospitalist oversees the patient journey in the hospital ward. These physicians take detailed histories and physicals pulling information from previous inpatient and outpatient encounters and noting any changes in the patient’s medical and social history. Hospitalists can have anywhere from 15-25 patients. So unfortunately, hospitalists might not have the time to perform a detailed review for each patient. While nutritional status is a concern for the patient, improvements in nutritional status is not something that can be fully resolved in a hospitalized visit and may require significant effort in the outpatient setting. Outpatient care falls outside the purview of the hospitalist.The Patient
Mr. Doe* is admitted and is treated with 80mg of Lasix, three times a day for his congestive heart failure. The patient’s cardiac echo from this year shows an ejection fraction (EF) of 15%. The hospitalist notes decreased medication compliance and increased water intake, but does not include any more information about food intake. He recommends that Mr. Doe consider going to hospice due to his advanced congestive heart failure (CHF). The patient continues to get daily labs. A nutritional assessment is completed by the dietitian for “length of stay” three days after admission. The nutrition assessment note does not identify any indicators from the nutritional risk screen. The only anthropometric traits measured are temperature and weight, recorded by a bed scale. BMI is calculated to be 19.8. The patient was placed on a cardiac diet.Takeaways from Treating Malnutrition in the Hospital
It is important to understand there are different etiologies of malnutrition that can be closely related to other common diagnoses treated in admitted patients. The top 5 ICD-10 diagnosis codes that are coded along with malnutrition are sepsis, acute kidney failure, pneumonia, pneumonitis, and hypertensive heart and renal disease with heart failure.¹ One would hope that the hospitalists’ clinical gestalt would ask more probing questions related to malnutrition and lead to a quicker consult to the dietitian. According to research in Austria, inpatient physician referrals to dietitians are only 16.8%.² Patients with medical issues such as cardiovascular disease and musculoskeletal disease were 2.2 times less likely to be referred to dietitians compared to patients with weight loss and low BMI.² With increasing awareness of different types of malnourished patients, the hope is this awareness will lead to improved physician referrals to dietitians in the inpatient setting. Documentation of malnutrition by dietitians can differ from documentation by clinicians. A healthcare system in Delaware found that out of the 291 cases of malnutrition diagnosed by dietitians, only 32% of these cases were diagnosed by clinicians.³
Hospital policy also matters. Per the Malnutrition Quality Improvement Initiative (MQii), a malnutrition toolkit devised by a national collective of dietitian nutritionists (RDNs) to help better diagnose malnutrition, hospitals should have a nutrition screening conducted on patients within 24 hours of admission.⁴ Additionally, nutritional screening policies can be structured to include as many cases as possible such as a borderline BMI, like this patient. While this patient did not have malnutrition diagnosed on this visit, you will see in Part 4 of this blog series, how diagnosis of malnutrition can differ between hospitals. It is important to note that after the diagnosis of malnutrition, care needs to be delivered in a timely manner. Gaps in care for malnutrition, whether that is communication, testing, or discharge related, leads to a 48% increase in length of stay.⁵What areas in this patient’s journey do you feel can be improved on?
Junum’s MalnutritionCDS™ software improves clinical workflows, saves physicians time, and drives hospital revenue. Our intuitive tools operate within existing EHR workflows, giving clinicians easy access to the nutrition insights they need to drive improved outcomes. Junum’s MalnutritionCDS™ increases the quality of malnutrition care and drives new top-line revenue along with providing a KPI data driven scorecard to track progress.
*To protect the patient’s identity, names and initials have been changed.
¹ Guenter P, Abdelhadi R, Anthony P, Blackmer A, Malone A, Mirtallo JM, Phillips W, Resnick HE. Malnutrition diagnoses and associated outcomes in hospitalized patients: United States, 2018. Nutr Clin Pract. 2021 Oct;36(5):957-969. doi: 10.1002/ncp.10771. Epub 2021 Sep 6. PMID: 34486169. ² Eglseer D, Bauer S. Predictors of Dietitian Referrals in Hospitals. Nutrients. 2020 Sep 18;12(9):2863. doi: 10.3390/nu12092863. PMID: 32962105; PMCID: PMC7551325. ³ Vest MT, Papas MA, Shapero M, McGraw P, Capizzi A, Jurkovitz C. Characteristics and Outcomes of Adult Inpatients With Malnutrition. JPEN J Parenter Enteral Nutr. 2018 Aug;42(6):1009-1016. doi: 10.1002/jpen.1042. Epub 2017 Dec 27. PMID: 29360158; PMCID: PMC6021228. ⁴ Silver HJ, Pratt KJ, Bruno M, Lynch J, Mitchell K, McCauley SM. Effectiveness of the Malnutrition Quality Improvement Initiative on Practitioner Malnutrition Knowledge and Screening, Diagnosis, and Timeliness of Malnutrition-Related Care Provided to Older Adults Admitted to a Tertiary Care Facility: A Pilot Study. J Acad Nutr Diet. 2018 Jan;118(1):101-109. doi: 10.1016/j.jand.2017.08.111. PMID: 29274640. ⁵ Ringel JB, Jannat-Khah D, Chambers R, Russo E, Merriman L, Gupta R. Impact of gaps in care for malnourished patients on length of stay and hospital readmission. BMC Health Serv Res. 2019 Feb 1;19(1):87. doi: 10.1186/s12913-019-3918-3. PMID: 30709377; PMCID: PMC6359768. -
Junum Releases Updated MalnutritionCDS™ Solution on Epic App Orchard
March 01, 2022Junum Releases Updated MalnutritionCDSTM Solution on Epic App Orchard
New clinical decision support tools can help physicians diagnose malnutrition early and intervene sooner

New Orleans, LA. (March 1, 2022): Junum, an innovative digital health company, is pleased to announce that version 2.0 of its MalnutritionCDS™ solution is now available on Epic’s App Orchard.
Junum’s solution integrates with the Epic EHR system to help hospitals better identify malnutrition, deliver exceptional patient care and maximize revenue capture.
In the US, one in three patients admitted to the hospital is malnourished or at risk — but <8.9% are diagnosed.¹ This latest Junum version introduces new features designed to help physicians spot this insidious condition early:
Clinical Decision Support Prompts notify physicians when patients meet diagnostic criteria for malnutrition so they can intervene sooner.
The Nutrition Summary saves physicians time by consolidating nutrition care data into a single view and automatically formatting progress notes with supporting information to clinically validate malnutrition diagnoses.
The Malnutrition Scorecard tracks key clinical, quality and financial indicators to help monitor and continuously improve malnutrition quality measures.
“Malnutrition diagnoses are often missed because providers don’t have the tools, workflows or training to identify it,” says Molly Hegarty, MS RDN, Founder and CEO of Junum. “That’s why we’re excited to introduce the Nutrition Summary – a consolidated, easy-to-digest view that’s an ideal sidekick to use during multidisciplinary rounds.”
Junum’s Clinical Advisor, Dr. Juan Ochoa, MD, FACS, FCCM adds, “Missed malnutrition diagnosis puts patients at risk for worse outcomes. One undervalued way for physicians to adapt and serve this patient population’s needs is to address nutrition aggressively at the beginning of their hospital stays.”
See the press release here
Media inquiries, please email sales@junum.ioAbout Junum
Junum is founded and led by Molly Hegarty, nutritionist and engineer. The company helps hospitals understand and address malnutrition to maximize the value of their clinical teams, drive revenue and deliver exceptional patient care. Our intuitive tools operate within existing EHR workflows, giving clinicians easy access to the nutrition insights they need to drive improved outcomes. Schedule a demo today at junum.io.Epic and App Orchard are trademarks or registered trademarks of Epic Systems Corporation. MalnutritionCDS and Junum are trademarks or registered trademarks of RDF Technology, LLC.
References
¹ Guenter P, Abdelhadi R, Anthony, P et al. Malnutrition diagnoses and associated outcomes in hospitalized patients: United States 2018. Nutr Clin Pract. 2021 https://doi.org/10.1002/ncp.10771 -
The Malnourished Patient Journey: Part 1 The ED
February 14, 2022By Samir Hussaini, MD
Join us on a four part blog series to explore a patient on his care journey and how malnutrition played an important role in his outcomes. Part 1 of our journey will walk you through the patient’s emergency department (ED) visit.
The Role of the ED Physician
The emergency department physician is the frontline provider of the patient care journey. These individuals are triaging patients based on their severity of illnesses and determining whether patient care needs to be upgraded to admission status. These physicians are primarily focused on making sure the patient does not deteriorate in an instant. Their time is limited and the patient’s nutritional status, while important to them, is a less prioritized concern. Below we will learn how nutrition taking a backseat in the ED can impact a patient.The Patient
Mr. Doe*, a 71 year old male with a history of congestive heart failure (CHF), coronary artery disease (CAD), hyperlipidemia(HLD), and hypertension (HTN), presents with shortness of breath. The patient’s vitals are borderline hypotensive and tachycardic. The ED physician completes a physical exam noting that he is a frail individual with crackles in his lungs and decreased breath sounds. The physician orders labs which show electrolyte derangement for sodium, potassium, and creatinine, and a brain natriuretic peptide (BNP) in the 3000s. The chest x-ray ordered shows an enlarged heart with congestion. The ED physician diagnoses Mr. Doe with an acute exacerbation of CHF needing admission and evaluation for heart failure.The Missing Link: What happened in the ED?
As one can see above, there was no mention or review of the patient’s nutritional status in the ED physician’s workup of the patient. Furthermore, the diagnosis and treatment of malnutrition is a difficult process to be done in the ED, in some part due to the goal of expedient care or transition of care. ED physicians usually do not consult dietitians in the ED and nutritional intervention is usually not performed in this setting. Lanctin et al extracted data from 950 hospital EDs across the nation looking at the prevalence of malnutrition diagnosed. The diagnosis prevalence of malnutrition has ranged from 0.7% in 2006 to 1.15% in 2014.¹ This is unfortunately an under diagnosis of malnutrition, as the diagnosis is around 8.9% rate based on the latest data made available by ASPEN.² Within reason, this could be a potential area where physicians can do better in assessing for signs of nutrition risk. One area for improvement is additional physician education about the under diagnosis of malnutrition and how assessing for nutrition risk factors in the ED may help with early diagnoses and interventions that can improve patient outcomes. A pilot study in Australia successfully implemented a model of care with screening and nutritional intervention in the ED.³ Twelve weeks after intervention these participants had weight gain, increase in quality of life, and decreased depression.³ Another avenue is making the EHR streamline data gathering to look at previous documentation with concern for malnutrition and making it plainly available to physicians in the ED.What would you have done differently to address malnutrition for this patient?
Junum’s MalnutritionCDS™ software improves clinical workflows, saves physicians time, and drives hospital revenue. Our intuitive tools operate within existing EHR workflows, giving clinicians easy access to the nutrition insights they need to drive improved outcomes. Junum’s MalnutritionCDS™ increases the quality of malnutrition care and drives new top-line revenue along with providing a KPI data driven scorecard to track progress.
*To protect the patient’s identity, names and initials have been changed.
References:
¹ Lanctin DP, Merced-Nieves F, Mallett RM, Arensberg MB, Guenter P, Sulo S, Platts-Mills TF. Prevalence and Economic Burden of Malnutrition Diagnosis Among Patients Presenting to United States Emergency Departments. Acad Emerg Med. 2021 Mar;28(3):325-335. doi: 10.1111/acem.13887. Epub 2020 Aug 31. PMID: 31724782. ² Guenter P, Abdelhadi R, Anthony P, Blackmer A, Malone A, Mirtallo JM, Phillips W, Resnick HE. Malnutrition diagnoses and associated outcomes in hospitalized patients: United States, 2018. Nutr Clin Pract. 2021 Oct;36(5):957-969. doi: 10.1002/ncp.10771. Epub 2021 Sep 6. PMID: 34486169. ³ Vivanti A, Isenring E, Baumann S, et al. Emergency department malnutrition screening and support model improves outcomes in a pilot randomised controlled trial. Emerg Med J 2015;32:180–3. -
Malnutrition A Hidden Epidemic in Older Adults
February 03, 2022Malnutrition in older adults is not so obvious. This population is particularly at risk, often from chronic conditions that leave them vulnerable to malnutrition.
The U.S. spends more than $51 billion in health care costs each year for disease-associated malnutrition in older adults. Why does this matter? Over 65% of hospitalized older adults could face malnutrition.
Older adults are at greater risk for malnutrition and poorer outcomes, including more frequent hospitalizations and increased likelihood of being in long-term care facilities.
Watch this short video to learn about malnutrition’s risk, impact on older adults, tips, and treatment and prevention.
-
The Albumin and Prealbumin Conundrum: Why Other Tools are Better Suited for Malnutrition Diagnosis
January 24, 2022By Samir Hussaini, MD
The Albumin and Prealbumin Conundrum
Why Other Tools are Better Suited for Malnutrition DiagnosisMalnutrition can double the length of stay of hospitalized malnourished patients compared to non-malnourished patients, and can be a complicated condition to diagnose. Without a widely accepted way to monitor and diagnose this condition, there has previously been too much emphasis on traditional laboratory markers, specifically albumin and prealbumin. Unfortunately, serum albumin and prealbumin may not be the most direct measure of nutritional status for malnutrition diagnosis. A better solution would be a nutrition-focused physical exam(NFPE) with vital input from registered dietitians to help diagnose malnutrition, a solution that can be easily facilitated with MalnutritionCDS™ software from Junum.
The start of albumin and prealbumin and its role in inflammation
The use of serum albumin to describe malnutrition was first written by Blackburn et al in 1977¹. Around that time, it was used as an instant assessment to identify those that would benefit from significant nutritional support. In 1995, prealbumin was seen as a more sensitive biomarker to measure nutrition and a patient’s response to nutritional support². This led to a 40-year old practice of using serum albumin and later prealbumin to identify malnutrition, but unfortunately this may not be the best marker for nutritional status.
While inflammation is a potential etiology of malnutrition, albumin and prealbumin are better measures for inflammation and are inappropriately used to measure direct nutritional status and to diagnose malnutrition. Davis et al found that there was no significant difference in change of serum prealbumin despite changes in protein and energy intake³. The only cause of change in serum prealbumin was an increase in C-reactive protein(CRP), a serum biomarker used to describe inflammation.
The sticky relationship between albumin and prealbumin with body composition
Serum albumin and prealbumin can be incorrectly used as proxy for measurement of muscle mass and body composition. It is understandably assumed that as one’s BMI decreases from malnutrition the serum albumin and prealbumin would drop as well. However, a study shows that decrease in serum albumin and prealbumin is seen once the patient reaches below a BMI of 12 while having six weeks or more of starvation⁴. It isn’t as straightforward as it seems.
Better tools to diagnose malnutrition
To better diagnose malnutrition, there are more accurate tools than solely using serum albumin and prealbumin. The recommended approach being the Academy of Nutrition and Dietetics and American Society of Parenteral and Enteral Nutrition (Academy-ASPEN) criteria, a comprehensive methodology being validated to diagnose malnutrition in the hospital setting⁵. This criteria does not take into account just serum albumin and prealbumin, but energy intake, weight loss, body fat, muscle mass, fluid accumulation, and grip strength. Some examples of what dietitians look for include:
- Eating less than 50% of estimated energy requirements for more than 5 days
- Noticeable muscle loss around the temple of the head
- Swelling of the lower legs
The best way to do this in the hospital setting is to include the registered dietitians in your treatment plan. The dietitians are the experts in understanding patient nutritional status and are the most qualified to use the Academy-ASPEN criteria in the process to diagnose malnutrition. Junum’s MalnutritionCDS™ software is the optimal solution in assisting dietitians to accurately record malnutrition in the hospital setting and give patients the best care they can.
References:
¹ Blackburn GA, Bistrian BR, Maini BS, Schlamm HT, Smith MF. Nutritional and metabolic assessment of the hospitalized patient. JPEN J Parenter Ent Nutr. 1977;1(1):11-21 ² Evans DC, Corkins MR, Malone A, Miller S, Mogensen KM, Guenter P, Jensen GL; the Use of Visceral Proteins as Nutrition Markers: An ASPEN Position Paper. Nutr Clin Pract. 2021 Feb;36(1):22-28. doi: 10.1002/ncp.10588. Epub 2020 Oct 30. Erratum in: Nutr Clin Pract. 2021 Aug;36(4):909. PMID: 33125793. ³ Davis CJ, Sowa D, Keim KS, Kinnare K, Peterson S. The use of prealbumin and C-reactive protein for monitoring nutrition support in adult patients receiving enteral nutrition in an urban medical center. JPEN J Parenter Enteral Nutr. 2012;36(2):197-204. ⁴ Lee JL, Oh ES, Lee RL. Finucane. TE Serum albumin and prealbumin in calorically restricted, nondiseased individuals: a systematic review. Am J Med. 2015;128(9):e1-1023.e22. ⁵ Hipskind P, Rath M, JeVenn A, Galang M, Nawaya A, Smith E, Lopez R, Cresci G. Correlation of New Criteria for Malnutrition Assessment in Hospitalized Patients: AND-ASPEN Versus SGA. J Am Coll Nutr. 2020 Aug;39(6):518-527. doi:10.1080/07315724.2019.1699476. Epub 2019 Dec 30. PMID: 31886743. -
Malnutrition Diagnoses and Associated Outcomes in Hospitalized Patients
January 21, 2022We have partnered with ASPEN on a short video to review key findings from the study, Malnutrition Diagnoses and Associated Outcomes in Hospitalized Patients: United States, 2018.
Did you know, those with a coded diagnosis of malnutrition (CDM) were:
- Significantly older
- In a lower community-level income category
- On Medicare as the payer
ASPEN has been tracking malnutrition-associated outcomes over the years using Agency for Healthcare Research and Quality (AHRQ) databases.
Watch the full video here: https://bit.ly/3fvuZBr
View and download our infographic that highlights study results found in the video.
-
Dietitians: Driving Revenue & Value in Hospital Malnutrition Care
November 16, 2021 By Ashley Matthews, MS, RD, LD, CNSC, PMP, Head of Clinical Excellence, Junum
By Ashley Matthews, MS, RD, LD, CNSC, PMP, Head of Clinical Excellence, JunumThere is no secret about the impact malnutrition has on patient outcomes. It is well known that dietitians add value via medical nutrition therapy for patients. One area that often gets overlooked is how dietitians add value by working to positively impact the patient and the hospital’s financial implications when treating malnutrition.
So, how do we link the value of patient care provided by dietitians to the financial bottom line?
Let’s start by explaining how the payor system works in the hospital setting.
Billing and coding are essential to the healthcare revenue cycle processes. They are the processes which translate a patient encounter into the languages used for claims submission and reimbursement.¹
According to CMS, a hospital’s case mix index (CMI) represents the average diagnosis-related group (DRG) relative weight for that hospital. It is calculated by summing the DRG weights for all Medicare discharges and dividing by the number of discharges.²
Hospital costs associated with malnutrition are related to the average length of stay. Medicare establishes the expected average length of stay based on the final Medicare Severity-Diagnosis Related Group (MS-DRG).³
So, how do we link the value of patient care provided by dietitians to the financial bottom line?
When malnutrition is identified, coded, and treated appropriately, the assigned MS-DRG may change, indicating a longer expected length of stay, thus, more appropriately capturing the resource requirements associated with providing care for malnourished patients.³
There are five ICD-10-CM codes for malnutrition that have been designated as either a major complication/co-morbidity (MCC) or complication/co-morbidity (CC) under the MS-DRG system.⁴ , ⁵
ICD-10 Code Description E43 Unspecified severe protein-calorie malnutrition (MCC) E44.0 Moderate protein-calorie malnutrition (CC) E44.1 Mild protein-calorie malnutrition (CC) E45* Retarded development following protein-calorie malnutrition (CC) E46 Unspecified protein-calorie malnutrition (CC) * Used in pediatric population
A major complication/comorbidity (MCC) or complication/co-morbidity (CC) may result in a higher Medicare payment to account for more intense levels of care and/or longer lengths of stay.³
Here is an example of the financial impact of properly diagnosing, documenting, and coding malnutrition care for a patient.
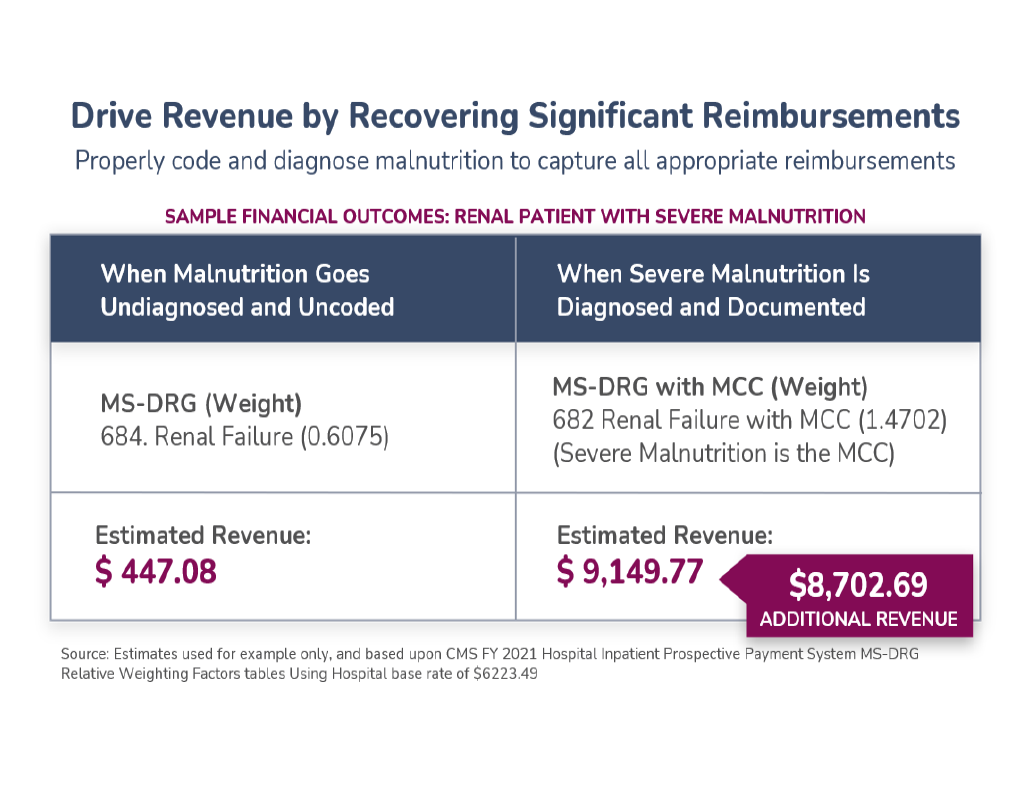
In order for hospitals to bill for the treatment of malnutrition on the basis of the severity of the condition (mild, moderate, or severe) and qualify for increased reimbursement from Medicare, a medical diagnosis by the physician must be accompanied by a plan of care that was implemented during the hospitalization.⁶ The plan of care for patients generally requires alignment between the dietitian and physician in malnutrition severity level with supporting evidence (e.g. AND/A.S.P.E.N. malnutrition criteria) and individualized nutrition interventions that are documented as part of the treatment plan.
Since ICD terminology fails to incorporate the impact of the inflammatory response on nutrition diagnosis, assessment and treatment, in 2012, the Academy and A.S.P.E.N. delineated an initial set of clinical characteristics to facilitate the standardized recognition and documentation of adult malnutrition by dietitians, Primary Care Providers (PCPs) and other members of the health care team (AND/A.S.P.E.N. malnutrition criteria).³
Dietitians play a critical role as the nutrition experts in utilizing clinical judgment along with the AND/A.S.P.E.N. malnutrition criteria to assess and document critical pieces of information used by PCPs, facility-based coders and others to validate a diagnosis of adult malnutrition (MS-DRG). Dietitians also provide medical nutrition therapy based interventions to improve the patient’s outcomes.
Tying it all together.
As a result of improvements in malnutrition diagnosis capture initiated by dietitians, hospitals may see a positive impact on their overall case mix index (CMI).
CMI is a key performance indicator for the hospital’s overall performance and clinical documentation practices. Having higher case mix index values indicate that a hospital has treated a greater number of complex, resource-intensive patients, and the hospital will be reimbursed at a higher rate.⁷
Conclusion: Yes, dietitians are a revenue generating department in the hospital setting.
References (Accessed on 10/06/2021):
¹ Trends in RDN knowledge and patterns of coding, billing and paymenthttps://www.eatrightpro.org/-/media/eatrightpro-files/news-center/in-practice/mntprovider/09-102019.pdf?la=en&hash=6D99E91333E2012B0D56B21F8C0193E3AAF44F66 ² Case Mix Indexhttps://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Acute-Inpatient-Files-for-Download-Items/CMS0226306 ³Consensus Statement of the Academy of Nutrition and Dietetics/A.S.P.E.N.: Characteristics Recommended for the Identification and Documentation of Adult Malnutrition (Undernutrition) (J Acad Nutr Diet. 2012; 112: 730-738https://www.jandonline.org/article/S2212-2672(12)00328-0/fulltext ⁴ Common Diagnoses (ICD-10-CM) Codes Related to Nutrition Serviceshttps://www.eatrightpro.org/-/media/eatrightpro-files/payment/medicare/nsc106-i---common-icd-10-cm-codes-related-to-nutrition-services.pdf?la=en&hash=0A68C07DE68D00FCD9602A78D73C5EA8B102B965 ⁵ Center for Medicare and Medicaid Services 2017 ICD-10-CM and GEMshttps://www.cms.gov/Medicare/Coding/ICD10/2017-ICD-10-CM-and-GEMs ⁶ State Operations Manual, Center for Medicare and Medicaid Serviceshttps://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/som107ap_a_hospitals.pdf ⁷ What is case mix index (CMI)https://www.definitivehc.com/resources/glossary/case-mix-index\#:~:text=This%20measure%20reflects%20the%20diversity,reimbursed%20at%20a%20higher%20rat For Academy of Nutrition and Dietetics Members, more information can be found in the “Malnutrition Codes - Characteristics and Sentinel Markers” section. https://www.eatrightpro.org/payment/coding-and-billing/diagnosis-and-procedure-codes/malnutrition-codes-characteristics-and-sentinel-markers
-
ASPEN Malnutrition Awareness Week
October 04, 2021
Junum is proud to help sponsor Malnutrition Awareness Week 2021.
Malnutrition Awareness Week™
Date: October 4-8, 2021
Website: https://www.nutritioncare.org/maw/
Join ASPEN, the American Society for Parenteral and Enteral Nutrition, for ASPEN Malnutrition Awareness Week on October 4-8, 2021.
It’s a week filled with valuable educational webinars and sharing of informational materials. Continuing education credit is available for most of the webinars that week. ASPEN is accredited to provide medical, pharmacy, nursing and dietetic credits.
The goal of Malnutrition Awareness Week is to educate healthcare professionals on early detection, prevention, and treatment of malnutrition; educate consumers/patients to discuss their nutrition status with healthcare professionals; and to increase awareness of nutrition’s role on patient recovery.
New Survey Announcement
We are excited to share Junum’s Hospital Malnutrition Quality Survey (HMQS). Our goal is to help you assess whether or not malnutrition care at your organization is clinician focused and provides enhanced data reporting through an optimized EHR.
Want to see how your hospital stacks up? Find out by taking the short survey here.
If you are curious to learn more about how Junum can help your hospital maximize the value of your clinical teams, drive revenue, and deliver exceptional patient care, watch our video. Don’t forget to subscribe!
Join the conversation online by using the hashtag #MAW2021. For more information and to register, visit www.nutritioncare.org/maw.
-
Putting Malnutrition Diagnoses Under the Microscope
September 14, 2021Tips for Documenting Findings (And Preparing for Audits)
By Ashley Matthews, MS, RD, LD, CNSC, PMP, Head of Clinical Excellence, Junum
There has been a lot of discussion lately around accurately coding for malnutrition. Just last year, the Office of Inspector General released a report casting doubt on hospitals’ ability to accurately document and diagnose this insidious condition.
Naturally, the Centers for Medicare and Medicaid Services (CMS) is paying attention and continues to conduct audits accordingly. And importantly, in recent listening sessions, members of the CMS Provider Compliance Division (CPD) met with members of ASPEN, the Academy, ASN and ACDIS to hear their concerns about improper denials and disputed criteria used by auditors. (This blog post from the director of ACDIS goes into more detail.)
In the end, CMS’ focus on malnutrition is good news. Nearly 30% of patients admitted to hospitals are at risk of malnutrition, but <7% are diagnosed.¹ The more focus this pervasive condition receives, the better. Still, audits can be nerve wracking and may even lead dietitians to second-guess their findings.
It is important to accurately document findings of malnutrition and evidence of treatment. Quality of care — and accurate reimbursements — often depend on it. So here are some tips to help you be more confident in your documentation and diagnoses.
Standardize Your Criteria
Whether your hospital uses AND/ASPEN, Merck Manual or GLIM criteria, it’s a good idea to choose one set of criteria and use it consistently. Clinical nutrition leaders should work with hospital leadership to standardize on a set of criteria based on modern, evidence-based standards, and make sure all providers and CDI team members are on board. Getting everyone on the same page can greatly reduce the burden placed on your coders, along with simplifying communication between providers and dietitians.Audit Yourself
Do your process improvement initiatives address malnutrition? The time to evaluate your processes is now — before external auditors do it for you. You can start today by auditing your workflows to make sure all pertinent team members are using the malnutrition diagnosis information from the chart in their documentation.Train and Train Again on the Nutrition-Focused Physical Exam
Regular training can keep new hires and long-term staff working from the same playbook when it comes to this critical exam. Now, you may be thinking these exams take too much time to conduct with all patients. Fair enough — but sound policies and procedures can help your team consistently identify patients who should have a full nutrition-focused physical exam and those who are well nourished enough to forego it.Own Your Value and Enter the Room
The COVID-19 pandemic has prevented many dietitians from entering patient rooms. At some hospitals, other care team members are doing their best to gather the information dietitians need to assess a patient and document their findings. However, dietitians should also be empowered to assert their value as essential staff alongside nurses and physicians. One way to do this is to find ways to enter patient rooms (if PPE is available) and do a physical assessment.And remember, Junum can help you simplify documentation, diagnosis and communication between dietitians and physicians. Our clinician-driven technology helps dietitians document signs and symptoms of malnutrition, select a severity level and alert physicians — all within existing EHR workflows. Contact us today and discover what better malnutrition diagnoses could mean for your hospital.
References
¹ Barrett ML, Bailey MK, Owens PL. Non-maternal and Non-neonatal Inpatient Stays in the United States Involving Malnutrition, 2016. ONLINE. August 30, 2018. U.S. Agency for Healthcare Research and Quality. Available: www.hcup-us.ahrq.gov/reports.jsp -
Remembering the Human in Healthcare Technology
August 27, 2021Key Takeaways From the HIMSS 2021 Conference
Whether you joined in person or online, this year’s HIMSS conference was a powerful opportunity to reflect upon the role technology has played throughout the COVID-19 pandemic.
Our industry pivoted to telehealth almost overnight — bringing with it a greater need for cybersecurity and support for remote workforces. Artificial intelligence (AI) technologies have helped us disseminate test results and communicate with patients in quarantine. And more advanced robotic process automation (RPI + AI) has been used to free up clinical staff and streamline services. At HIMSS, everywhere you turned was another example of digital transformation improving the delivery of healthcare.
During the HIMSS Digital session entitled “The Future of Healthcare,” it was exciting to see how health systems, payers, clinicians, patients and health/IT providers have all focused on digital health and transformation in their own ways. And yet, according to the 2021 HIMSS State of Healthcare Report, we still face significant challenges to clinical adoption.
Let’s look at a few key take-aways:
- 92% of clinicians have recommended the use of digital health tools for their patients
- 78% of clinicians believe that the pandemic has resulted in helpful changes like the adoption of virtual care, telehealth, etc.
- Yet only 57% of clinicians believe that digital health tools are user friendly and easy to learn
Clearly, clinicians support our industry’s digital transformation. So why are nearly half of them having difficulty with the resulting innovations?
Barriers to Adoption
According to the report, there are several important factors keeping them from adopting new technology more readily:
- 61% of clinicians cited a lack of interoperability between IT systems
- 41% have concerns about patient data security
- 39% note that new innovations don’t fit into their current workflows
Clearly, lack of technology is not the issue. But in order for our innovations to deliver their full value, we must make life easier for the user — especially when that user is an overtaxed clinician in the throes of a global pandemic.
Keeping Humans at the Heart of our Innovations
At this year’s HIMSS, the human element was perhaps more visible than ever before. Whether in conference rooms or through our computer screens, we united as human beings passionate about improving healthcare through technology. And for those of us working at the intersection of patient care and tech, it was just what we needed.
At Junum, we are focused on technology innovation that automates nutrition care workflows while making sure nutrition data is accessible to everyone — patients, caregivers and clinicians. Schedule a demo today to learn how we can help your hospital.
-
Junum featured in 5 Top Healthcare Startups Impacting Nutrition from StartUs Insights
June 08, 2021“Staying ahead of the technology curve means strengthening your competitive advantage. That is why StartUs Insights gives you data-driven innovation insights into the healthcare sector. This time, you get to discover 5 hand-picked startups developing solutions impacting Nutrition.”
Read the article: Discover 5 Top Healthcare Startups impacting Nutrition
-
What is a Feasibility Assessment?
June 01, 2021The Challenge
Malnutrition is a concern at hospitals everywhere. And its true impacts — both clinical and financial — are too often hidden by lack of data. While EMRs are highly effective for many clinical use cases, they aren’t often designed to support nutrition care partnerships between physicians and dietitians — including identifying and diagnosing malnutrition.The Solution
Junum developed the MalnutritionCDS™ solution to help hospitals accurately diagnose malnutrition within their existing EHR workflows — and improve revenue capture accordingly. But before the technology is implemented, hospitals must fully understand the problem malnutrition presents — and the opportunities available for improvement.“The true clinical and financial impacts of malnutrition can be difficult to quantify because many hospitals track malnutrition data manually, if they track it at all,” explains Molly Hegarty, Founder and CEO of Junum. “That’s where we come in — to help hospitals understand what’s possible with better malnutrition data, processes and technology, and then make it a reality.”
Junum approaches this exercise in a structured, efficient and data-driven way. It’s called a feasibility assessment. Here’s how it works, and why it’s important.
What is a Feasibility Assessment?
During this critical process, Junum works with hospital stakeholders to identify the greatest opportunities for improvement by comparing their current malnutrition workflows to evidence-based clinical guidelines and best practices. It typically lasts approximately six weeks.How Does It Work?

We start with in-depth interviews and workflow observations to understand current malnutrition care practices and identify opportunities for improvement — from admission to discharge. This may include data points such as:- Nutritional workflows
- Clinician notes templates
- System alerts
- Query templates
- Case mix index
- ICD-10 reports (DRG, CC/MCC)
- Billing denials
- Clinician training protocols
- Patient assessments
- Food intake tracking
- Various internal reports related to malnutrition
- Nutritional case management
A steering committee is established with key stakeholders to provide well-rounded input and feedback. Roles may include:
- Clinical Nutrition Manager
- Physician Champions
- SVP of Care Coordination
- CDI/Coding Manager
- AVP of Information Technology
- VP/SVP Innovation
Identifying Opportunities for Impact

Next, we analyze the learnings from the clinical discovery phase and identify areas where Junum can help the hospital make the greatest impact. While this is different for every hospital, our clients have worked with us to:Capture Missed Reimbursements
Our clients have nearly doubled their malnutrition diagnosis rates — and seen multi-year revenue increases as a result.Improve Malnutrition Coding to Reduce Payer Denials
When physicians and CDI team members can easily access RD notes, they can support better documentation, earlier intervention and more appropriate reimbursements.Enable Earlier Assessment
By adding a validated screening tool like MST to nursing workflows, hospitals can significantly increase RD referrals for nutrition assessments.Innovating a Path Forward: Digital Transformation and Software Implementation

Now that we understand the clinical and financial opportunity of improving malnutrition care, we can do something about it. Using learnings from the feasibility assessment, Junum outlines a digital transformation plan for the hospital. This involves agreeing upon financial models and KPIs to track progress, and documenting deliverables and risks. Once approved, Junum will implement its MalnutritionCDS software to help the hospital make an impact on the metrics that matter.A “Blind Spot” No More
“Our MalnutritionCDS solution helps hospitals better diagnose malnutrition and maximize the clinical and financial outcomes that come along with that. By doing a feasibility assessment first, we can hone in on the specific opportunities that will help each hospital or health system do that most effectively,” explains Hegarty. “There’s no need to rely on educated guesses or predictions — we can lay out their real-world opportunities in black and white. It’s a powerful way to bring the hidden impact of malnutrition to light.”At Junum, we have successfully guided many hospitals through this process, and we’d love to do the same for yours. Contact us at sales@junum.io to get started.
-
Junum Announces MalnutritionCDS™ Integration with Epic EHR
May 18, 2021Junum Announces MalnutritionCDS™ Integration with Epic EHR
Easy-to-access nutrition insights help hospitals better diagnose malnutrition and maximize revenue
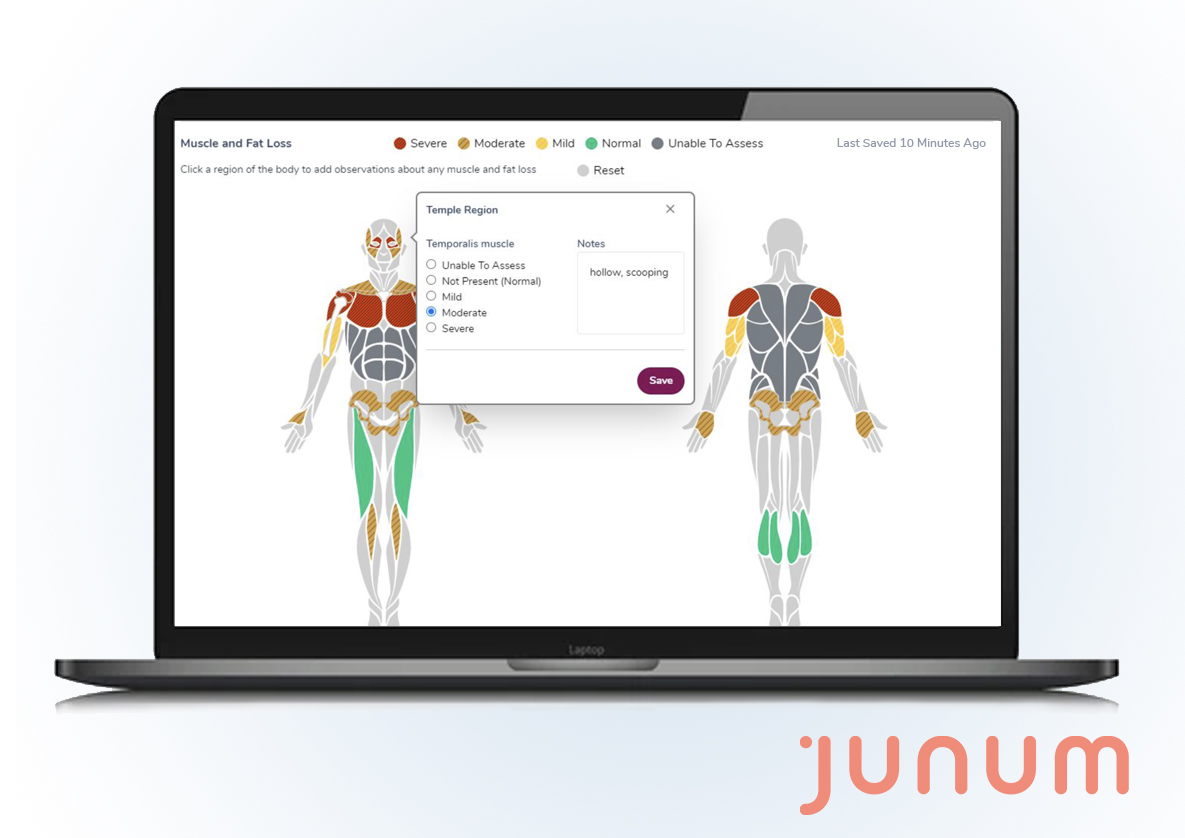
New Orleans, LA. (May 18, 2021): Malnutrition is a common, complicated, and costly problem for hospitals. In the US, one in three patients admitted to the hospital is at risk for malnutrition — but <8.9% are diagnosed.(1) Junum developed its MalnutritionCDS™ solution to help hospitals address this critical “blind spot,” deliver exceptional patient care and maximize revenue capture.
And today, Junum is pleased to announce that its MalnutritionCDS solution is now available on Epic’s App Orchard. View the listing here.
A Clinical Nutrition Solution for Solving Malnutrition in the Hospital
Built using the latest FHIR-based API technology, Junum’s solution integrates with the Epic EHR system to deliver the nutrition insights physicians need to accurately diagnose malnutrition — all within their existing EHR workflows.
The tool guides dietitians through the nutrition-focused physical exam, helping identify and document evidence of malnutrition severity to:
- Inform clinical decisions by putting nutrition insights in front of physicians in the EHR — early and at a glance
- Improve patient care by better diagnosing and documenting malnutrition early enough to inform care plans
- Maximize revenue by recovering significant reimbursements
A Clinical Solution with Financial Impact
When malnutrition is properly diagnosed and coded, reimbursements can rise significantly. In fact, hospitals using Junum’s solution have nearly doubled their malnutrition diagnosis rates — and seen multi-year revenue increases as a result.
“When care teams can diagnose malnutrition early, they can intervene sooner to help improve patient outcomes and capture the appropriate reimbursements,” says Molly Hegarty, MS RDN, Founder and CEO of Junum. “As an engineer turned nutritionist, I believe strongly in using the power of technology to help clinicians better understand nutrition and its vital role in patient care. We’re excited to make our SMART on FHIR, malnutrition-focused app for clinicians available to Epic users across the country.”
See the press release Here
Media inquiries, please email sales@junum.io
About Junum
Junum is founded and led by Molly Hegarty, nutritionist and engineer. The company helps hospitals understand and address malnutrition to maximize the value of their clinical teams, drive revenue and deliver exceptional patient care. Our intuitive tools operate within existing EHR workflows, giving clinicians easy access to the nutrition insights they need to drive improved outcomes. Schedule a demo today at junum.io.
Epic and App Orchard are trademarks or registered trademarks of Epic Systems Corporation.
MalnutritionCDS and Junum are trademarks or registered trademark of RDF Technology, LLC.
References
Barrett ML, Bailey MK, Owens PL. Non-maternal and Non-neonatal Inpatient Stays in the United States Involving Malnutrition, 2016. ONLINE. August 30, 2018. U.S. Agency for Healthcare Research and Quality. Available:www.hcup-us.ahrq.gov/reports.jsp
-
A Day in the Life of Junum's CEO
January 26, 2021 Molly Hegarty, is the founder and CEO of Junum. She is a former Intel engineer turned Registered Dietitian and Licensed Dietitian Nutritionist with over 10 years of experience in clinical nutrition. Her career began in technology but shifted to clinical nutrition after experiencing a personal tragedy when her college roommate passed away from Crohn’s disease related complications. She witnessed firsthand the value of nutrition in the critical care setting.
Molly Hegarty, is the founder and CEO of Junum. She is a former Intel engineer turned Registered Dietitian and Licensed Dietitian Nutritionist with over 10 years of experience in clinical nutrition. Her career began in technology but shifted to clinical nutrition after experiencing a personal tragedy when her college roommate passed away from Crohn’s disease related complications. She witnessed firsthand the value of nutrition in the critical care setting.Molly saw the silos and gaps across the healthcare system that existed due to a lack of cohesive, supporting nutrition-focused technology. Molly decided to refocus her career path from direct clinical care to using her tech expertise to create software that would help to make a difference. Her passion motivates other people who share that vision to work with her on this mission to put nutrition on the forefront of healthcare.
There is no typical day for Molly at Junum. As a startup founder with a completely remote team, daily priorities can shift quickly. Junum was a 100% remote team prior to Covid and everyone was hand selected for the expertise that they bring to the team. Molly stays connected with her team through Slack, email, Zoom, and Google Meet. Every day each team member posts a daily standup in Slack. This helps to ensure everyone is unified on tasks across teams. Molly reviews her calendar first thing in the morning, checks the team slack messages, and goes through her emails. This enables her to set priorities for the week and manage her time efficiently.
To keep her vision for Junum on track, Molly maintains a running task list for each team with priority items that are shared with the entire organization. This encourages an environment of transparency, accountability, and teamwork. It is not uncommon for team members to lend a hand to different departments in need. Monday’s are typically meeting heavy and begin with a full Junum team meeting to go over her priority list and get team updates on open tasks. By holding these team meetings on Mondays, it frees Molly up to spend the rest of her week doing other important tasks like meeting with investors, working with the advisory board, hosting informational webinars, reviewing budgets, checking in with customers, or attending a conference. Although her day never looks the same, Molly is always up for the challenges of a health tech startup. To help stay grounded, Molly takes yoga breaks or tea breaks throughout the day and allows time to recharge herself for the next task.
The Junum team is focused in many areas this year. The main focus is providing optimal support to our existing customers as well as generating new sales. Previously the sales team focused on east coast hospital systems, but now that reach has expanded to systems across all regions of the US. There is also focus this year to expand the team. The team expansion will further Junum’s progress in implementing its technology solution to disrupt traditional malnutrition care in the acute care environment.
 Covid has impacted all of us in so many ways personally and professionally. In terms of work, it means getting better at building digital relationships and engaging customers through webinars and other virtual events. (Molly wrote a whole article about this–see Springboard blog article.) In terms of team building, Covid has presented many challenges. Before Covid, Junum would have in person staff retreats to help foster relationships. Since Junum is a nutrition company - the employee retreats always have the best food. Unfortunately, Covid has forced these retreats to be put on hold, but Molly is looking forward to many more employee retreats in new locations with fantastic food. In the meantime, Molly makes sure there are thoughtful, special events to break up the monotony of the Covid routines for the employees. She fosters the remote team relationships by holding bi-weekly “Tea Time’’ zoom calls to just chat among employees and catch up on life without mentioning work. This has been a great way to build friendships and learn more about the team. It’s important to have social time to build relationships.
Covid has impacted all of us in so many ways personally and professionally. In terms of work, it means getting better at building digital relationships and engaging customers through webinars and other virtual events. (Molly wrote a whole article about this–see Springboard blog article.) In terms of team building, Covid has presented many challenges. Before Covid, Junum would have in person staff retreats to help foster relationships. Since Junum is a nutrition company - the employee retreats always have the best food. Unfortunately, Covid has forced these retreats to be put on hold, but Molly is looking forward to many more employee retreats in new locations with fantastic food. In the meantime, Molly makes sure there are thoughtful, special events to break up the monotony of the Covid routines for the employees. She fosters the remote team relationships by holding bi-weekly “Tea Time’’ zoom calls to just chat among employees and catch up on life without mentioning work. This has been a great way to build friendships and learn more about the team. It’s important to have social time to build relationships.Covid has pushed Molly to find a good balance between taking care of her home, prioritizing self care, and fostering relationships with friends and family in new ways. Although she does miss travel for work and for personal travel adventure, she is thankful not to spend so much away from home. She much prefers her own cooking to airport food!
Molly is excited that 2021 is a year where health systems are focusing on the importance of technology that actually benefits physicians instead of creating more work for them. Digital health technology that is made correctly should reduce pain points for physicians and improve the clinician experience. Molly is proud that Junum is a new way for physicians and other providers to embrace technology that helps improve patient outcomes in a way that saves clinician time and improves patient outcomes. It is amazing for Junum to be part of such a big shift in the way care is delivered. For more information about Junum please contact our sales team at sales@junum.io.
-
New Investment and Upcoming Webinar
January 05, 2021Malnutrition (a nutrient imbalance, deficiency or excess) is an ongoing issue in healthcare linked to higher infection rates, longer lengths of stay and increased risk of mortality—all with devastating impacts on hospital revenue and overall patient outcomes. Malnutrition is a common, complicated, and costly problem for hospitals. Insufficient tools and disconnected care processes make it difficult for hospitals to grasp and fully address the issue. In fact, 20-50% of patients experience malnutrition in the hospital setting, yet only 5-10% are diagnosed. Junum’s technology helps hospitals address the critical “blind spot” of nutrition in patient care today.
Junum works by helping hospitals understand and address malnutrition to maximize the value of their clinical team and deliver exceptional patient care. Our intuitively-designed tools operate within existing EHR workflows, giving clinicians easy access to nutrition insights that drive improved outcomes. Junum’s physician tool increases revenue and reduces risk by improving quality through real-time clinical decision support and malnutrition tracking.
Jumpstart Foundry Invests in Junum
The Jumpstart Foundry (JSF) recently announced the second round of 2020 portfolio selections. JSF enables and empowers the most promising innovations in health. More than 200 startup companies applied and only five were selected for the Fall 2020 cohort.
Junum is excited to be included in the Fall 2020 cohort along with Butterflly Health (behavioral health solution), Patient Forecaster (emergency medicine AI-powered advanced labor management platform), TeloPoint (care management), and RevKeep (post payment medical audits).






The JSF is a Nashville-based venture capital firm that is excited to Make Something Better in health. Each year, the JSF invests in 20-25 innovative health companies that are expected to have a major impact in the health domain and drive strong financial returns for Jumpstart’s investors. Each startup company that is selected to participate in a cohort is guided and supported through JSF’s systematic, step-by-step process. These companies are connected with Jumpstart’s network of industry experts.They will also participate in the Jumpstart Refinery which is a JSF exclusive digital community for networking that supports growth acceleration.Learn more about Junum:
Our Founder & CEO, Molly Hegarty, MS, RD, LDN will host a free informational webinar on Thursday, January 21 at 1pm EST.
Molly is a former Intel engineer and a Registered Dietitian. Her nationally recognized unique technical and clinical expertise empowered her to develop our efficient, effective digital healthtech solutions.
Sign up here: http://bit.ly/JunumJanWebinar
We look forward to helping you improve malnutrition care at your facility using our technology.
Read the Jumpstart Foundry Announcement here:
-
ASPEN Malnutrition Awareness Week
November 08, 2020
Junum is proud to help sponsor Malnutrition Awareness Week.
Malnutrition Awareness WeekTM
Date: October 5-9, 2020
Website: www.nutritioncare.org/mawJoin ASPEN, the American Society for Parenteral and Enteral Nutrition, for ASPEN Malnutrition Awareness Week on October 5-9, 2020.
It’s a week filled with valuable educational webinars and sharing of informational materials. Continuing education credit is available for most of the webinars that week. ASPEN is accredited to provide medical, pharmacy, nursing and dietetic credits.
The goal of Malnutrition Awareness Week is to educate healthcare professionals on early detection, prevention, and treatment of malnutrition; educate consumers/patients to discuss their nutrition status with healthcare professionals; and to increase awareness of nutrition’s role on patient recovery
Join the conversation online by using the hashtag #MAW2020. For more information and to register, visit www.nutritioncare.org/maw.
-
TMCx Demo Day 2019
May 18, 2020TMCx Demo Day for digital health drew a standing-room-only crowd to the Texas Medical Center Innovation Institute on June 6, 2019 to hear presentations from the 19 companies in the TMCx08 cohort.

Malnutrition is insidious, and, coupled with a focus on treating the patient’s presenting illness, often goes unrecognized in patients presenting to the hospital or clinic. Malnutrition leads to numerous complications and prolonged recovery times. Junum is making great strides in stopping this vicious pattern. TMC Innovation is proud to call Junum a part of its community knowing that the founding team understands the nuances and complexities of malnutrition. Junum’s technology seamlessly integrates into the caretakers’ workflow eliminating barriers of implementation. Junum empowers the user to coordinate complex malnourishment cases while capturing the value of care rendered. Companies like Junum need to be a part of everyday medicine as we focus our efforts to deliver higher quality healthcare at a lower cost.
–Lance Black, MD, MBID – Associate Director, TMCx
Read the article: TMCx Demo Day offers digital health solutions for urgent issues.
-
State of Care: Evolving Industry Video
May 01, 2020 -
Make America Healthy Again
April 15, 2020Written by: Margaret Dittloff, MS RDN
While we await the official results of the 2020 election, let’s examine this Stat News commentary “Make America Health Again” about the lack of health care policy and support for nutrition despite the fact that nutrition is a critical component of everyone’s health and wellbeing. Dr. Rahman and Mr. Ross point out that “the majority of Americans (are) being both overfed with unhealthy foods and undernourished with healthier ones.” Nutrition has been under valued and under-represented in America’s healthcare systems. They highlight the following suggestions for our next administration:
- Refocus research on nutrition
- Make health food more affordable and unhealthy food less affordable
- Teach doctors about nutrition
- Provide food assistance program incentives for healthy eating
- Use the bully pulpit & hold food industry accountable (especially in ads and merchandizing techniques)
I would also add that we need CMS and private payers to cover and fully reimburse the nutrition services of Registered Dietitians (RDNs). Dietitians are the trained healthcare professional experts in food and nutrition who can help provide that nutritional guidance that doctors are missing.
Lastly, we need we need better nutrition data in EHRs to help alert doctors to their patient’s nutritional problems. But we need that nutrition data to be structured and interoperable (something I’m exceedingly passionate about) to it can follow the patient and flow between consumer health apps and different EHR systems.
-
ICD10monitor Podcast Talk Ten Tuesdays
April 01, 2020ICD10monitor’s popular Talk Ten Tuesdays show reports on current issues related to medical coding, clinical documentation integrity (CDI) and payment methodologies to help providers in all settings. In this week’s show, Molly Hegarty MS RD, founder and CEO of Junum, reports on possible revenue loss when the presence of a malnutrition diagnosis is not documented appropriately, and Dr. McClain Blanton, a physician advisor with the Brundage Group, reports on the clinical aspects of the study.
Beyond CCs and MCCs: Say Hello to HCCs and APR-DRGs



































